As margins tighten, traditional revenue cycle management strategies are on shaky ground. Many healthcare providers are turning to automation and AI to simplify payments, prevent revenue loss and protect profits. This article breaks down some of the most common revenue cycle management (RCM) challenges facing healthcare leaders and offers a practical checklist to optimize patient access, collections and claims management, while building a resilient and patient-centered revenue cycle.
Common challenges in revenue cycle management
Revenue cycle management is how healthcare organizations handle the financial side of patient care, from patient billing to claims management. Healthcare providers rely on RCM to ensure they are properly paid, so they can keep the lights on, pay their staff and deliver quality patient care.
Are traditional RCM strategies still fit for purpose? Consider some of the current challenges:
- Patients are responsible for a larger share of costs due to high-deductible health plans. How can providers help them understand their financial obligations and make it easier to pay without hurting their experience?
- Minimizing claim denials is a daily focus, thanks to constantly changing policies and regulatory updates. How do revenue cycle teams keep up with payers?
- Staffing shortages remain on the agenda. How can providers ease pressure on staff to maintain productivity and morale?
- There’s also the question of how to turn mountains of data into actionable insights. How do teams interpret it correctly to identify bottlenecks and opportunities for improvement?
Automation and AI offer a way through. When implemented thoughtfully, these tools can speed up processes, reduce errors and clear operational roadblocks for a more resilient revenue cycle. The following revenue cycle management checklist includes some of the key questions to consider along the way.
Checklist for improving revenue cycle management
Automating patient access
- Can patients book appointments online?
- Does the online scheduler automate business rules to guide patients to the right provider?
- Are patient identities verified at registration and point of service?
A healthy revenue cycle starts with efficient patient access. According to the State of Patient Access 2024, 60% of patients want more digital options for scheduling appointments, managing bills and communicating with providers. Providers who see improvements in patient access also credit automation, which speeds up intake and improves accuracy.
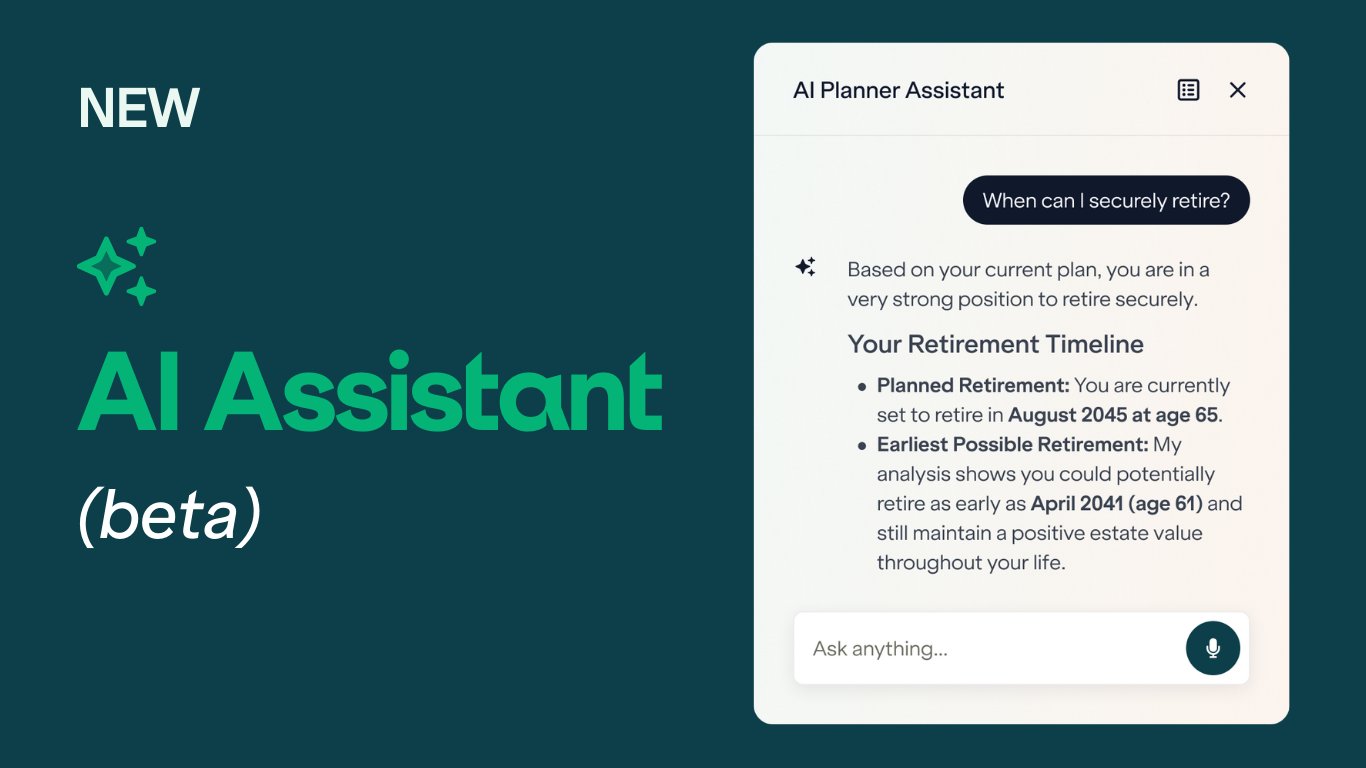
A good first step is to replace paper-based processes with online self-scheduling and self-service registration. These tools make life easier for patients, boosting satisfaction, retention and engagement. Behind the scenes, Experian Health’s new AI-powered tool, Patient Access Curator, helps providers get paid faster by verifying and updating patient information with a single click – accelerating registration and paving the way for faster reimbursement.
Optimize patient collections with data and analytics
- Are patient estimates provided upfront?
- Are notice of care requirements being addressed?
- Are patients offered appropriate financial plans and easy ways to pay?
With more financial responsibility resting on patients’ shoulders, patient collections are under the spotlight. The State of Patient Access report shows that upfront estimates and clarity about coverage are top priorities for patients, because when they know what they owe, they’re more likely to pay on time. Implementing tools to promote price transparency and easy payment methods should feature in any RCM checklist.
WithCoverage Discovery, healthcare organizations can run checks across the entire revenue cycle to find billable commercial and government coverage that may have been forgotten, to maximize the chance of reimbursement. Meanwhile, Patient Payment Estimates offers patients clear, accessible estimates of their financial responsibility before treatment, so that hose who need financial assistance can be directed automatically to payment plans and charity options.
Case study: How UCHealth secured $62M+ in insurance payments with Coverage Discovery®
Improve claims management to reduce denials
- Are high-impact accounts prioritized?
- Are remittances reconciled with payments received?
- Does claims management software generate real-time insights and reports?
With 73% of healthcare leaders agreeing that denial increased in 2024, and 67% saying it takes longer to get reimbursed, claims management is a great use case for automation. ClaimSource®, ranked Best in KLAS in 2024 for claims management, automates the entire claims cycle in a single application. It integrates national and local payer edits with custom provider edits to verify that each claim is properly coded before submission. By focusing on high-priority accounts, providers can target resources in the most effective way to ensure a higher first-pass payment rate.
A major advantage for ClaimSource users is access to AI Advantage. This tool utilizes AI to “learn” from an organization’s historical claims data and trends in payer behavior to predict the probability of denial. It also segments denials so staff can prioritize those that are most likely to be reimbursed, reducing the time and cost of manual appeals and rework.
Benefits of implementing a revenue cycle management checklist
The key to choosing the right RCM tools and technologies is to build the strategy around what patients need most. A clear, transparent and compassionate billing experience is more manageable for patients and helps providers get paid faster. An RCM checklist helps teams stay focused on the tasks that matter.
Providers can build on the suggestions above by choosing the key performance indicators (KPIs) that align with their specific goals. Metrics like financial performance, billing efficiency and collections rates can be combined to guide resource allocation, drive improvements and speed up reimbursement. With a well-designed checklist informed by clear KPIs, revenue cycle leaders can keep their teams on track and take their organizations from “surviving” to “thriving.”
Learn more about how Experian Health’s revenue cycle management tools can help healthcare providers meet current challenges, improve the patient experience and increase cash flow.
Publisher: Source link