Health insurers are seeking steep premium increases on the Affordable Care Act’s exchanges next year, according to a new analysis from KFF.
The researchers examined rate filings from 312 payers participating in the marketplaces in all 50 states and the District of Columbia, and found a median proposed increase of 18%. That is 11 percentage points higher than requests submitted last year.
The last time payers requested similarly high premium increases was in 2018, when the “repeal and replace” effort in Congress created uncertainty in the policy arena. Now, the fallout from the One Big Beautiful Bill Act and the likely expiration of enhanced premium subsidies at the end of this year are clouding the outlook for exchange payers.
The findings track with KFF analysts’ expectations based on a look at early filings, where the median proposed increase was 15%.
“Uncertainty over federal policy changes has forced insurers to make some assumptions when developing their rates for 2026,” the researchers said.
Most proposed increases fall between 12% and 27%, according to the study, with 66 insurers proposing increases between 15% and 20%. Fifty-eight payers proposed increases between 10% to 15%, and 39 are requesting increases between 20% and 25%.
In addition, 30 payers are pitching premium hikes of between 25% and 30%, according to the study.
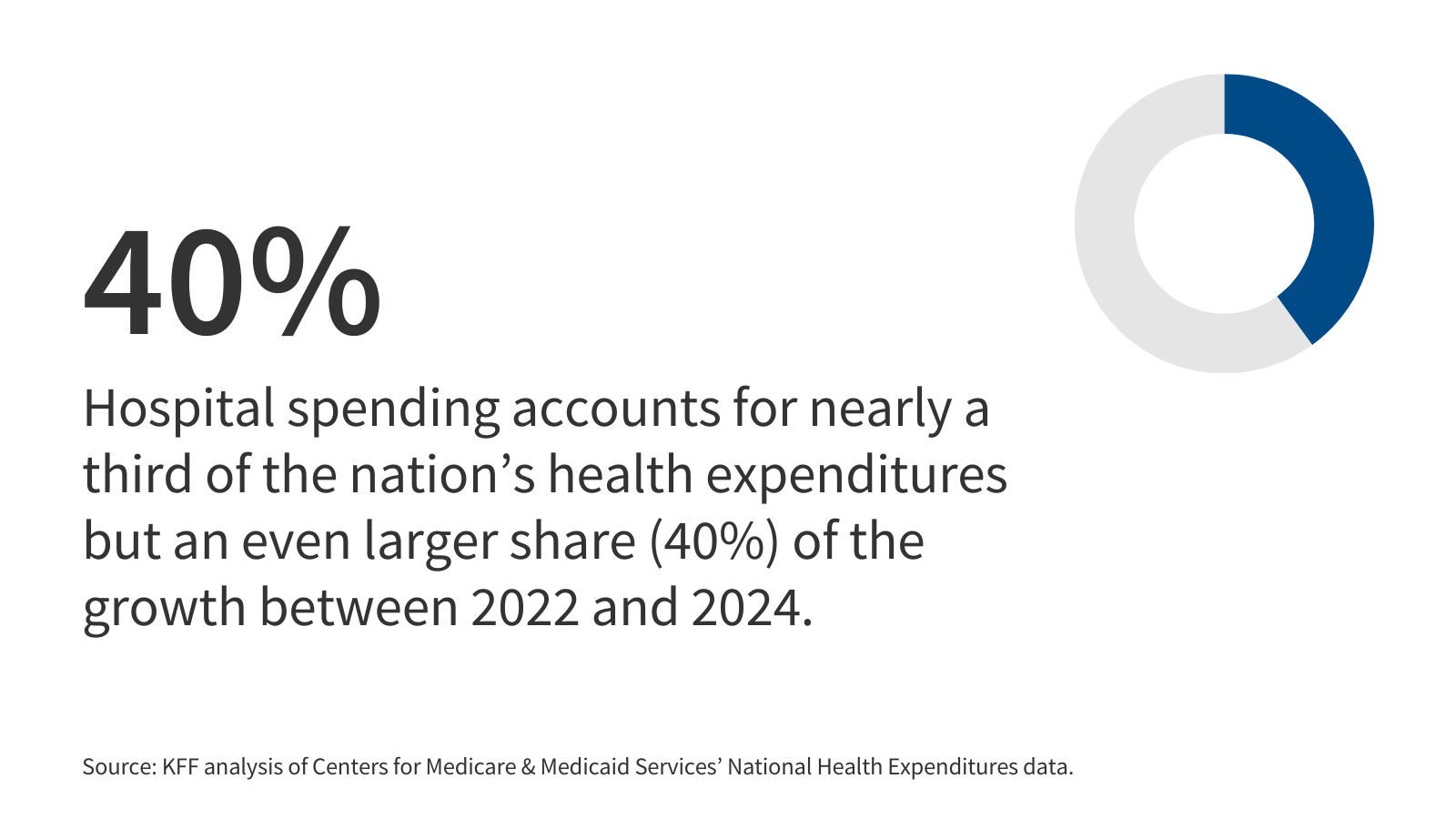
The study details the key factors that insurers are citing in their rate filings, with many noting medical cost trend as a critical driver. KFF said that, generally speaking, payers expect the cost trend to be in line with 2025, which was about 8%. However, some of the largest, publicly-traded companies have warned that costs are accelerating in this market.
Insurers also cited increasing labor costs, provider consolidation, tariffs and the demand around specialty drugs—particularly GLP-1s—as playing a role in proposed premium increases.
While the fate of the enhanced premium tax credits is still up in the air, most payers expect them to expire at the end of this year, which they predict could lead to significant changes in the member mix for 2026. On average, premium increase proposals were four percentage points higher than they would have been otherwise to account for this shift, according to the report.
“UHC anticipates a decline in enrollment due to higher post-subsidy premiums,” the insurer wrote in filings for a Maryland-based HMO plan, Optimum Choice. “Healthier members are expected to leave at a disproportionately higher rate than those with significant healthcare needs, increasing market morbidity in 2026.”
Some insurers have calculated rate increases for both scenarios, KFF said. Neighborhood Health Plan of Rhode Island, for example, proposed a 16% premium increase if the enhanced subsidies remain in place, which rises to 21% assuming they expire.
Publisher: Source link