The brief’s key findings are:
- Long-term care (LTC) costs are generally not well insured, posing a significant risk for older households as they age.
- Using new survey data, the analysis compares what respondents say they would do if LTC costs exceeded their resources to what people like them actually do.
- The key results are:
- many plan to rely on Medicaid, but, in reality, only a small fraction will meet its strict eligibility criteria;
- in contrast, people do not expect to tap home equity, but typically end up doing so; and
- among those who do need LTC services, few find it necessary to move in with their kids, but they do expect to leave them less money.
Introduction
Even the best-laid plans can go awry. Retirees face the risk of a large healthcare spending shock for medical or long-term care (LTC) either because their health insurance involves significant cost sharing or because they lack insurance entirely in the case of LTC. If these shocks are big enough, they can devastate a household’s finances. The question is how do retirees respond when faced with expenditures that exceed their resources?
This brief, which is based on a recent paper, addresses retirees’ responses in two steps.1 The first reports the results of a recent survey on how older households perceive medical and LTC risks in retirement and how they plan to respond if their resources prove inadequate. The analysis then turns to the Health and Retirement Study (HRS), a large longitudinal survey, to determine how households actually respond following a major healthcare expenditure.
The discussion proceeds as follows. The first section describes the extent to which individuals are insured for healthcare shocks. The second section summarizes the survey results on individuals’ perceptions of possible costs and how they might respond if resources are insufficient. The third section describes the data and methodology for the HRS analysis, and the fourth section presents the results. The final section concludes that while retirees are relatively well-insured against medical shocks – with implications seemingly limited to reductions in expected bequests – they are very exposed to unexpected LTC expenditures, often leading to a drawdown of home equity or reliance on Medicaid.
Insurance against Healthcare Risks in Retirement
In this brief, we use “healthcare” to refer to any health-related costs, whether they involve periodic medical care or long-term care. Starting off with medical costs, Medicare covers nearly all adults ages 65+, and about half had a Medicare Advantage plan in 2021 (see Figure 1).2 The remainder typically have a combination of Traditional Medicare and supplemental coverage either from an employer (current or previous), a Medigap plan, or Medicaid. Only 5 percent of those over 65 are covered solely by Traditional Medicare. Given the extensive coverage, retirees’ exposure to costs occurs through the extent of cost-sharing they face under the different arrangements. While such cost-sharing can be substantial in Traditional Medicare, the vast majority of retirees have some form of supplemental arrangement that can reduce the burden.
Even with supplemental insurance to augment Medicare, cost-sharing for doctor and hospital services typically involves some copay or coinsurance. While annual costs are capped by supplemental plans and Medicare Advantage (though not in Traditional Medicare), those caps may still leave households exposed to thousands of dollars of annual costs. In 2024, Medicare Advantage plans were required to cap annual costs to enrollees at $8,850 for in-network services and $13,300 for out-of-network services; and, since many households are married couples, the household cap is effectively doubled for them.3
Another source of uninsured expenditure – for the period covered in the following HRS analysis – is prescription drugs. Medicare drug coverage initially included substantial gaps, and supplemental plans in those years also often did not cover drugs. Moreover, when the Part D drug benefit was added to Medicare in 2006, retirees still faced a “donut hole” of thousands of dollars a year of drug costs that were uncovered until they hit “catastrophic” levels of spending (after which they still faced a 5-percent coinsurance rate). Recently, the donut hole and cost sharing for catastrophic coverage were eliminated, but these costs are important for the sample period in this analysis.
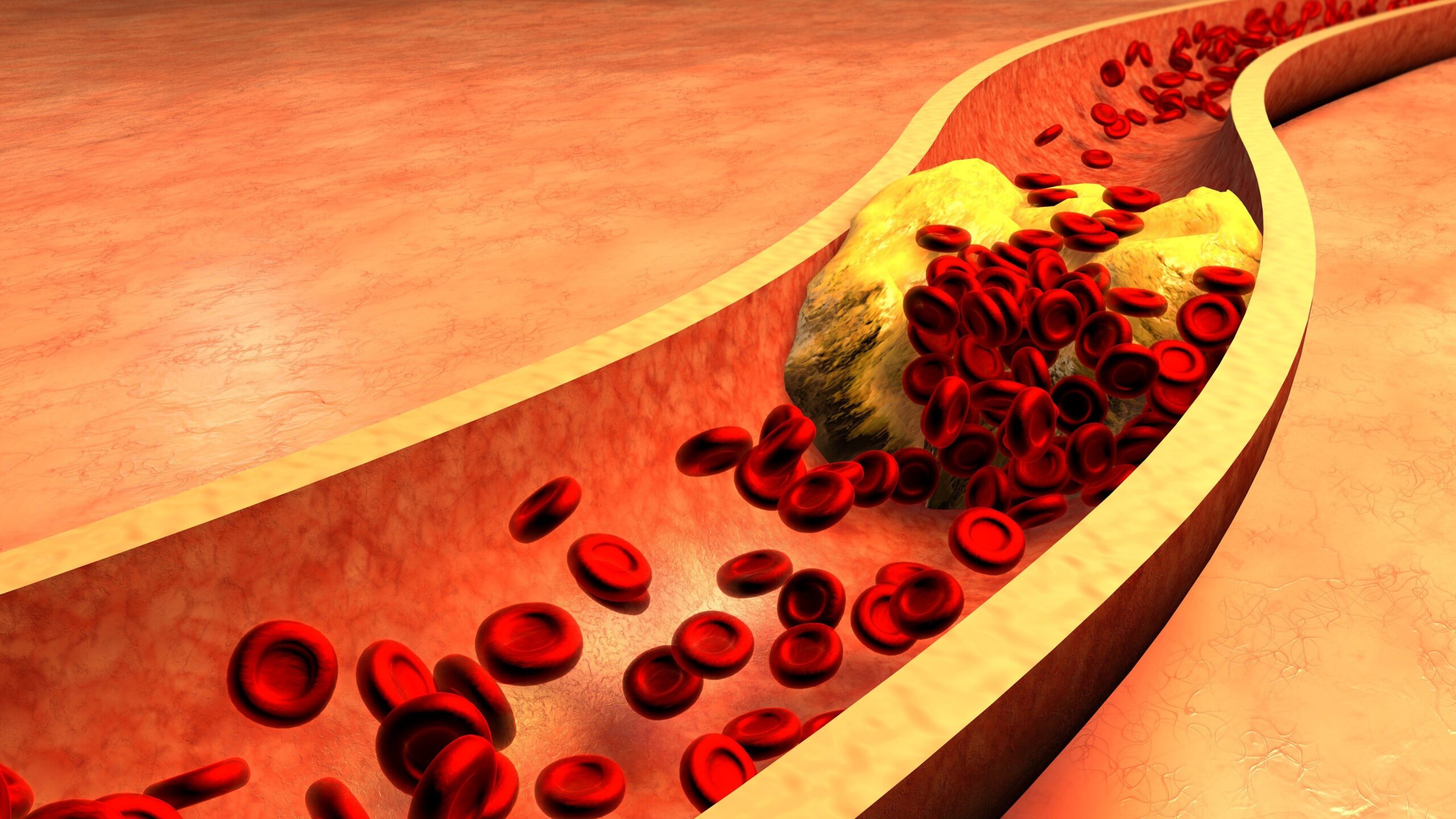
While retirees are fairly well protected against the cost of medical shocks, they are exposed to substantial LTC risks. About 80 percent of those ages 65+ will require some LTC, with nearly 20 percent requiring high-intensity care for more than three years.4 But only 4 percent of the hours required is covered by insurance (see Figure 2).5
The rest is covered primarily by informal care from family members, and the lion’s share of paid care is eventually covered by Medicaid. However, Medicaid eligibility requires the household to be impoverished. In 2024, the income limit for Medicaid eligibility for those over age 65 was typically around $2,800 per month ($5,600 for couples) and the asset limit was typically $2,000 ($3,000 for couples), but varies by state. Thus, Medicaid is a safety net, but not an effective form of insurance, since its deductible is virtually all a household’s assets.6 The lack of insurance for formal care is troubling, given that the median annual costs in 2023 were $116,800 for a private room in a nursing home, $64,200 for an assisted living facility, and $75,500 for home health aides.7
In sum, retirees are exposed to moderate medical spending – mostly capped at around $20,000 per year for a married household with Medicare Advantage. While no small sum, it is unlikely to completely derail a household’s long-term finances, although it may require adjustments (particularly as many medical conditions persist for years). In contrast, the costs of LTC can easily overwhelm household finances with just a few years of intensive care.
The economics literature on how retirees fare financially in the wake of a healthcare spending shock is surprisingly limited. In an attempt to fill that gap, the following reports the results of a recent household survey on people’s perceptions of possible shocks and their fallback plans if resources are inadequate. These results are then supplemented with findings from the HRS describing what actually happens to retirees in the wake of a healthcare shock.
Survey Results
In July 2024, Greenwald Research interviewed online 508 individuals ages 48-78 with at least $100,000 in investable assets. All the respondents were involved in the financial decision-making of their households. The survey asked participants about their perceived likelihood of experiencing a medical shock or needing extensive LTC, as well as the potential cost of these events. A key finding, consistent with other studies, was that medical and LTC risks were generally low on their list of concerns (see Figure 3).8 Moreover, responses to detailed questions in the recent survey about the likelihood of needing care and the cost of that care reinforce the notion that older adults underestimate the risks and costs.
Underestimating the risks of large outlays for healthcare means that households will not have adequate insurance or financial resources to cover such needs if they arise. When asked what alternatives they would consider if they could not afford their healthcare expenses, over 60 percent said they would consider spending down to Medicaid, while only 30 percent said they would consider using their home equity or moving in with their children (see Figure 4). The question is to what extent are these alternatives reasonable? To answer that question, the analysis turns to the HRS.
HRS Analysis – Sample and Methodology
The HRS is a biennial survey representative of the U.S. population over age 50 and their spouses. This analysis limits the sample to the Medicare-covered population ages 65+ and, to be consistent with the recent online survey, focuses on those with $100,000+ in investable assets. Although all respondents are initially non-institutionalized when first interviewed, they are tracked and re-interviewed even as they enter nursing homes and other institutions. Furthermore, the HRS includes questions on healthcare expenses by type: doctors, hospitals, prescription drugs, outpatient surgery, and dental costs on the medical front; and nursing home care and home care on the LTC front.
These healthcare expenses are used to define “medical shock” and “LTC shock.” Individuals are considered to have had a medical shock in a given year if spending was in the top 10 percent of medical out-of-pocket expenses in that year. For LTC, because out-of-pocket spending is relatively rare, a shock is defined as having any LTC-related spending. Individuals with multiple years of high spending are considered to have had the shock in the first year, with the subsequent years viewed as related to the initial event. This process yields nearly 1,500 unique individuals in the LTC shock group and around 4,000 in the medical shock group. All amounts are inflated to 2023 dollars.
The analysis explores four ways in which a large healthcare expense could affect an individual’s life. The first, and probably the most important, is the decision to enroll in Medicaid. The second is any impact on household assets – overall, residential, and non-residential – with an eye toward assessing if the shock leads to downsizing to fund the expense. The third involves a change in living arrangements, such as moving in with children to more easily receive care. Finally, a large healthcare expense could affect an individual’s expectations about leaving a bequest.9
To analyze the effects of shocks, one must contend with the fact that the households bearing such large costs are not similar to those without shocks. They may have had poorer health their whole lives, lack sufficient insurance coverage due to preexisting conditions or a lack of resources, or simply have different risk preferences. Such differences are hard to control for statistically in a regression. To address this problem, the analysis compares those who experience a shock in a given year to those who will experience the shock at some time in the near future.10 The expectation is that an individual with a large healthcare expenditure in a specific year should be similar on all manner of unobservable characteristics to one hit by the same shock just a few years later, if the precise timing of such shocks is close to random.
Thus, the analysis involves matching the group of individuals suffering a shock with a “control” group of individuals experiencing the same type of shock four years later. In this manner, the effects of the shock can be estimated at the time of impact, and up to two years later.11 Once the “shock” groups and control groups are defined, a regression equation is used to estimate the impact of the shock – LTC or medical – on the four outcomes – Medicaid, wealth, living with children, and bequest expectations.
HRS Analysis – Results
The section begins with a look at the characteristics of the survey participants, followed by the results for the analysis of healthcare shocks.
Descriptive Data
Before looking at how people respond to large financial shocks, some descriptive data relating to the sample and to the magnitude of the healthcare expenditures provide a useful backdrop. Table 1 presents the mean demographics for the two “shock” groups. These two samples are both broadly similar, except that those suffering an LTC shock have a mean age of 82 compared to 76 for those with a medical shock. In addition, the medical-shock group tends to have somewhat more education, higher wealth and, correspondingly, greater expectations of leaving large bequests.12
Table 2 displays mean out-of-pocket (OOP) costs in the year of the shock for those with an LTC shock and those with a medical shock. Overall, annual costs are quite high and similar for both samples – about $11,000. The standard deviation (SD) of these costs is also large – an individual who is one standard deviation above the mean would face nearly $30,000 of expenses in the shock year.13 Roughly two-thirds of LTC expenses are nursing homes, while within medical care, about half of expenses are for prescription drugs. This latter finding is not surprising given that many of these shock years occurred before Medicare Part D, and all before the elimination of the donut hole in the standard Part D benefit. Interestingly, while the medical group has much higher medical than LTC spending, the converse does not hold for the LTC sample. That group actually faces higher medical than LTC costs, showing that individuals facing large LTC expenses typically also bear large medical expenses at the same time.
Impact of Long-term Care Shocks
With this context in mind, Figures 5 through 7 show the impacts of an LTC shock on a variety of outcomes.14 First and most striking, Figure 5 shows that the share of individuals covered by Medicaid increases dramatically, by 6.6 percentage points, in the year of the LTC shock, and increases yet again the following year to 9 percentage points above the comparison group. These increases are enormous in relation to the baseline rate of Medicaid coverage in this population of 4 percent before the shock. Furthermore, prior to the shock, the shock and control groups move in parallel, as evidenced by the lack of significant differences in years -4 to -1. Thus, these findings suggest that the LTC shock was the reason for the increase in Medicaid enrollment.
Medicaid, however, is not a good solution for most households, since it requires the household to forfeit virtually all its wealth. Indeed, another recent study of ours found that only about 15 percent of households with $100,000+ in investable assets will actually end up on Medicaid.15 So, it is quite surprising that 61 percent of respondents in the recent survey said that they would consider spending down assets to qualify for Medicaid. At the same time, few survey respondents expected to tap their home equity to cover costs. In fact, though, the net worth of households hit by an LTC shock declined in the year of the shock by $78,200, relative to the comparison group. And the estimated decline in the value of the primary residence in Figure 6 suggests households do draw down their home equity to finance LTC shocks.16
Another way individuals can finance LTC is by reducing the amount they set aside for bequests. Some economists have argued that bequests are a luxury good (a good that people buy disproportionately more of as their income increases) and, as such, holding assets in reserve for bequests if individuals do not need much LTC is complementary to using such reserves to finance that care.17 The results are consistent with this model: the individuals in the analysis reduce their expected probability of leaving bequests of $100,000+, as a result of an LTC shock (see Figure 7). The decline is modest in magnitude, at 4 percentage points, but such probability questions are notoriously insensitive as respondents tend to round their answers substantially.18
Finally, some comfort can be taken in the fact that the results show no evidence that individuals who suffer an LTC shock move in with their children or move closer to their children (or that their children move closer to them). This pattern is consistent with the distinct preference of respondents in the survey to only move in with their kids as a last resort.19
In sum, individuals seem to have three main methods of absorbing LTC shocks in practice: drawing down wealth (particularly their home equity); possibly as a consequence, reducing their intended bequests, at least for modest bequest sizes; and falling back on the quintessential safety net, Medicaid. All of these results are qualitatively similar when the sample is not restricted to households with $100,000+ in financial assets.20
Impact of Medical Shocks
In contrast to the impacts of LTC shocks, the impacts of medical shocks are actually very limited. No statistically significant impact is found on any of the outcomes, with the exception of the expected chance of leaving a bequest of $100,000+ (see Figure 8), which is marginally significant at the 10-percent level.
Overall, the results provide suggestive evidence that households are fairly well-insured against medical shocks. This finding is in sharp contrast to LTC shocks, which is puzzling given that the magnitude of the financial hit in the year of the shock is similar for both types of shocks. A possible explanation is the persistence of shocks – while a medical shock is likely predictive of some future expenses, an LTC shock is much more likely to indicate a permanently elevated level of future expenditures. This difference in expected future costs is compounded by the fact that health insurance is never exhausted, while LTC insurance typically has lifetime limits.21
Conclusion
Insurance rarely offers full protection from risk, and in the case of healthcare risks, these shortcomings can be substantial. Large OOP healthcare expenditures are an indication of a lack of adequate insurance, either entirely (typical in the case of LTC) or on the margin (typical of cost-sharing in health insurance for medical care).
The analysis shows that individuals plan to rely on Medicaid, the main safety net program for healthcare, if their insurance proves inadequate. The results also confirm that Medicaid is, in fact, the major recourse of individuals struck by LTC shocks, for which private insurance coverage is rare. However, in the end only 15 percent of the population ends up on Medicaid, at least within the first couple of years after a shock. Instead, while survey responses suggest that people do not expect to draw down home equity to deal with healthcare expenses, the results of the HRS analysis show that tapping equity is actually a typical response to LTC shocks. Such shocks also lead to reductions in expected bequests.
In contrast to LTC, medical expenses seem well-insured, particularly in the sense that one bad year does not predict extraordinarily high-cost future years. Furthermore, health insurance does not typically feature lifetime limits, in contrast to LTC insurance (and Medicare coverage for close LTC substitutes such as extended hospital stays). Accordingly, the results suggest that the only major adjustment by individuals hit with a medical spending shock is a decline in expected bequests.
Overall, the results speak to the relative lack of protection retirees have against LTC shocks, and underscore the importance of Medicaid as a payer of last resort for those who develop LTC needs at older ages.
References
American Association for Long-term Care Insurance. 2020. “Long-Term Care Insurance Facts- Data- Statistics- 2020 Reports.” Westlake Village, CA.
Belbase, Anek, Anqi Chen, and Alicia H. Munnell. 2021. “What Resources Do Retirees Have for Long-Term Services and Supports?” Issue in Brief 21-15. Chestnut Hill, MA: Center for Retirement Research at Boston College.
Boccuti, Cristina, Gretchen Jacobsen, Kendal Orgera, and Tricia Neuman. 2018. “Medigap Enrollment and Consumer Protections Vary Across States.” Issue Brief. San Francisco, CA: Kaiser Family Foundation.
Chen, Anqi, Alicia H. Munnell, and Gal Wettstein. 2025a. “An Overview of Healthcare Risks in Retirement.” Special Report. Chestnut Hill, MA: Center for Retirement Research at Boston College.
Chen, Anqi, Alicia H. Munnell, and Gal Wettstein. 2025b. “Do Retirement Investors Accurately Perceive Healthcare Risks, and Do Advisors Help?” Working Paper 2025-3. Chestnut Hill, MA: Center for Retirement Research at Boston College.
Chen, Anqi, Alicia H. Munnell, and Gal Wettstein. 2025 (forthcoming). “How Do Retirees Cope with Uninsured Healthcare Costs?” Working Paper. Chestnut Hill, MA: Center for Retirement Research at Boston College.
De Nardi, Mariacristina, Eric French, and John B. Jones. 2010. “Why Do the Elderly Save? The Role of Medical Expenses.” Journal of Political Economy 118(1): 39-75.
Fadlon, Itzik, and Torben Heien Nielsen. 2021. “Family Labor Supply Responses to Severe Health Shocks: Evidence from Danish Administrative Records.” American Economic Journal: Applied Economics 13(3): 1-30.
Freed, Meredith, Jeannie Fuglesten Biniek, Anthony Damico, and Tricia Neuman. 2024. “Medicare Advantage in 2024: Premiums, Out-of-Pocket Limits, Supplemental Benefits, and Prior Authorization.” Issue Brief. San Francisco, CA: KFF.
Genworth Financial. 2023. “Cost of Care Survey.” Wellesley Hills, MA.
Gruber, Jonathan and Kathleen M. McGarry. 2023. “Long-Term Care in the United States.” Working Paper 31881. Cambridge, MA: National Bureau of Economic Research.
Hendren, Nathaniel. 2013. “Private Information and Insurance Rejections.” Econometrica 81(5): 1713-1762.
Hou, Wenliang. 2020. “How Accurate are Retirees’ Assessments of their Retirement Risk?” Working Paper 2020-14. Chestnut Hill, MA: Center for Retirement Research at Boston College.
Hubbard, R. Glenn, Jonathan Skinner, and Stephen P. Zeldes. 1995. “Precautionary Saving and Social Insurance.” Journal of Political Economy 103(2): 360-399.
Jones, John Bailey, Maracristina De Nardi, Eric French, Rory McGee, and Rachel Rodgers. 2020. “Medical Spending, Bequests, and Asset Dynamics around the Time of Death.” Economic Quarterly 106(4): 135-157.
Lindstrom, Rachel, Katherine Keisler-Starkey, and Lisa Bunch. 2024. “Percentage of Older Adults with Both Private Health Insurance and Medicare Decreased from 2017 to 2022.” Washington, DC: U.S. Census Bureau.
Lockwood, Lee M. 2018. “Incidental Bequests and the Choice to Self-Insurance Late-Life Risks.” American Economic Review 108(9): 2513-2550.
Ochieng, Nancy, Jeannie Fuglesten Biniek, Meredith Freed, Anthony Damico, and Tricia Neuman. 2023. “Medicare Advantage in 2023: Premiums, Out-of-Pocket Limits, Cost Sharing, Supplemental Benefits, Prior Authorization, and Star Ratings.” Issue Brief. San Francisco, CA: KFF.
Poterba, James, Steven Venti, and David Wise. 2011. “The Composition and Drawdown of Wealth in Retirement.” Journal of Economic Perspectives 25(4): 95-118.
RAND. Health and Retirement Study Longitudinal File, 1992-2020v2. Santa Monica, CA.
Tolbert, Jennifer, Patrick Drake, and Anthony Damico. 2023. “Key Facts about the Uninsured Population.” Issue Brief. San Francisco, CA: KFF.
University of Michigan. Health and Retirement Study, 1992-2020. Ann Arbor, MI.
Endnotes
Publisher: Source link