Medicare Advantage benchmark payments are poised to increase by 2.23%, the Centers for Medicare & Medicaid Services proposed in a Friday afternoon advance notice.
The rate hike represents a significant increase year-over-year from the federal government to MA health plans, compared to the previous year’s 0.16% dip.
Payments from the federal government to MA plans will increase by $21 billion, or 4.33% on average. Implementation of the MA risk adjustment model will also continue, the agency said.
“CMS has worked to ensure that people with Medicare Advantage and Medicare Part D have access to stable and affordable offerings,” said CMS Administrator Chiquita Brooks-LaSure in a news release. “Today’s advance notice continues CMS’ efforts to provide access to affordable, high-quality care in Medicare Advantage while being a good steward of taxpayer dollars.”
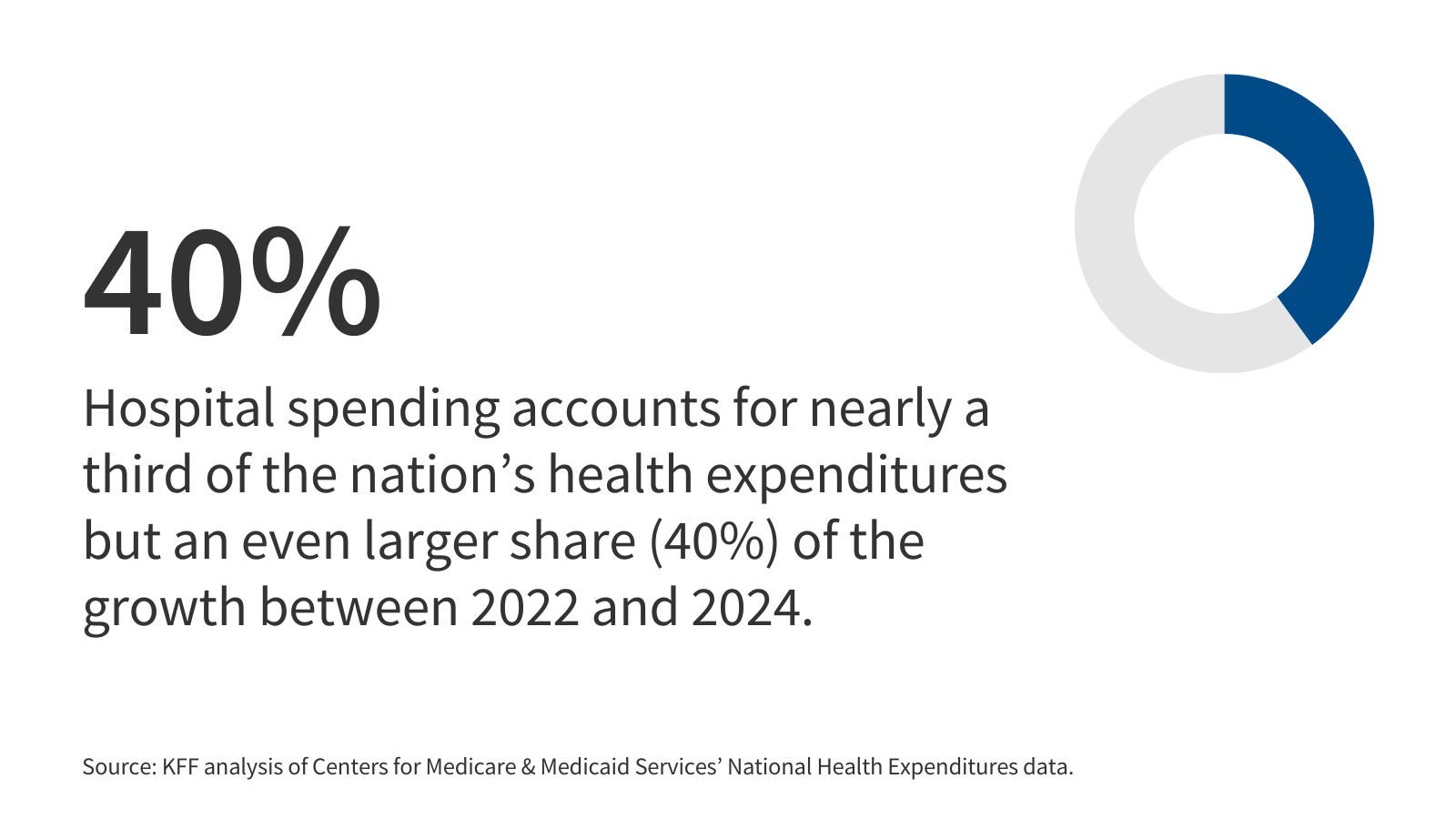
The government said it expects to spend $9.2 trillion over the next decade on MA payments to health plans. About $1.3 trillion will be utilized for supplemental benefits and premium buy-downs. CMS chose not to pause growth rates related to medical education costs or the risk adjustment model phase-in, which would have resulted in $10.4 billion more for MA plans in 2026.
Since the MA program is stable—with premiums, supplemental benefits and coverage options staying similar since last year—these changes were not necessary, CMS explained.
Most insurers were not happy at CMS when it followed through with a 0.16% cut to MA benchmark payments. At the time, CMS said the average payment increase was 3.7% and a $16 billion increase over the previous year.
Today’s announcement appears to be more favorable toward national payers. UnitedHealth, CVS Health, Humana and Centene stock all rose in after hours trading.
“This expected increase includes consideration of the various elements that impact MA payment, such as growth rates of underlying costs, 2025 Star Ratings for 2026 quality bonus payments, continued phase-in of risk adjustment model updates that were implemented in CY 2024 and CY 2025, and increases to risk scores because of MA risk score trend, which can be driven by a number of factors including MA demographics and coding patterns,” the agency said in a fact sheet.
Starting Jan. 1, annual out-of-pocket prescription drug costs are capped at $2,000 for enrollees. The cap increases to $2,100 for 2026.
CMS is accepting comments on the proposal until Feb. 10.
Publisher: Source link