On July 4, President Trump signed into law a budget and tax bill that includes significant changes to the Medicaid program including new requirements for states to implement work requirements for individuals enrolled through the Affordable Care Act (ACA) Medicaid expansion pathway or certain state waivers. The Congressional Budget Office (CBO) estimates that this requirement will have the largest effect on spending and coverage compared to other provisions, reducing federal Medicaid spending by $326 billion over ten years and resulting in 5.3 million more people who are uninsured.
In the summer of 2025 while the new law was under debate in Congress and shortly after enactment, the 25th annual budget survey of Medicaid officials in all 50 states and the District of Columbia conducted by KFF and Health Management Associates (HMA), in collaboration with the National Association of Medicaid Directors (NAMD) was in the field. To better understand how states are preparing for Medicaid work requirements, the survey asked states to discuss anticipated challenges to implementing work requirements by the end of 2026, including related system changes and data matching. KFF anticipates that work requirements will apply to 43 states (41 expansion states including the District of Columbia plus Georgia and Wisconsin, which have expanded Medicaid through waivers). We received responses to this question from 42 of these states.
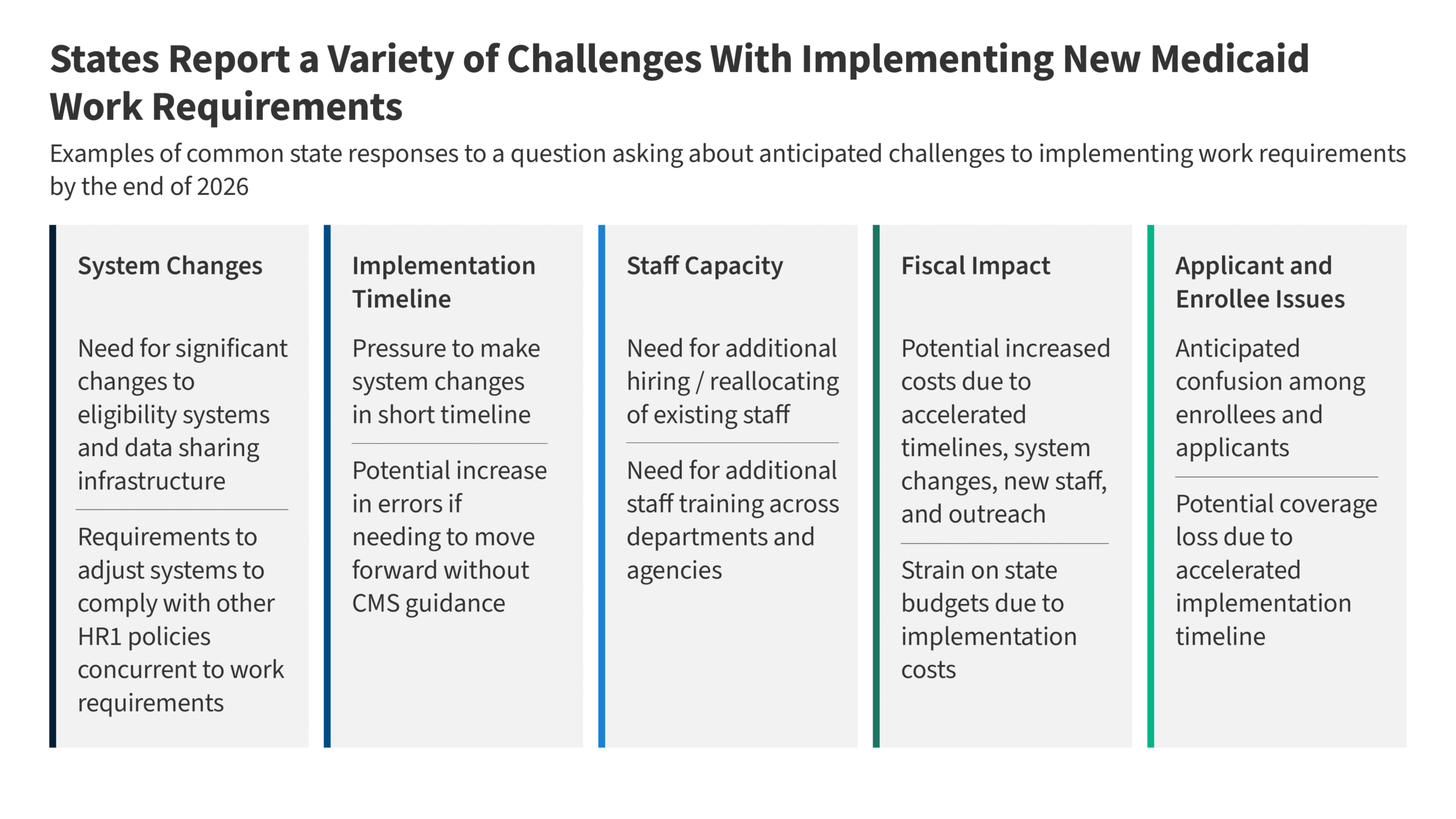
Because the survey question asked specifically about challenges pertaining to systems, nearly all states described system changes they expect to make; however, they identified other challenges as well. These challenges include how quickly the requirements must be implemented, staff capacity concerns, cost concerns, and issues for applicants and enrollees (Figure 1). In many cases, states described multiple, interrelated challenges. For example, the compressed implementation timeframe and need for federal guidance often factored into state responses detailing other challenges. Some states expressed more challenges than others. A few states that had already been pursuing 1115 waivers to implement work requirements reported fewer anticipated implementation challenges. Understanding state challenges can help inform the content and timing of forthcoming federal guidance.
States cited the need to make major changes to eligibility systems in a short timeframe and the need for enhanced data sharing infrastructure as major challenges. States will need to make significant changes to eligibility systems to be able to verify compliance with work, school, and other qualifying activities as well as to identify individuals who qualify for mandatory exemptions and optional exceptions. States expressed concern over having to make such major system changes in a very short timeframe, noting the long lead times typically needed to design, procure, and build new systems. Adding to the challenge will be the need to make key system design and workflow decisions before CMS releases guidance. Another priority many states mentioned is enhancing capabilities to collect and match data from multiple agencies and external sources (e.g., SNAP, Medicaid claims data, state education enrollment data) to reduce the burden on applicants and enrollees for documenting their work or exemption status (Figure 2). However, some states acknowledged that data sharing infrastructure is limited and establishing interfaces to accurately share data will take time to put in place.
According to several states, other policy changes in the law, including restrictions on eligibility for lawfully present immigrants, 6-month eligibility redeterminations for expansion enrollees, and limits to retroactive Medicaid coverage, also require significant systems changes. Increasing this complexity, some states also mentioned the challenge of aligning different work requirements across Medicaid, SNAP, and TANF, as well as having to make complex systems and eligibility policy changes for SNAP as required by the new law. These changes may be particularly complicated for states with integrated Medicaid and SNAP eligibility systems. In addition, a few states noted that they are currently involved in multiyear IT systems projects and that it will be challenging to complete those projects successfully while also simultaneously adding new systems redesigns. All of these systems challenges are further exacerbated by limited state staff capacity and financial resources.
According to many states, the short implementation timeline means they will need to move quickly with key systems changes and policy decisions before clear federal guidance is available. States have just over a year to prepare to implement work requirements on January 1, 2027, and have less than a year before they will need to begin outreach to notify individuals of the new requirements in September 2026 (Figure 3). The law directs the Secretary of HHS to issue an interim final rule on implementing work requirements by June 1, 2026, leaving little time between when the guidance is released and when outreach begins. For many states, this short timeline intensifies the pressure to move quickly with system upgrades, particularly given the often lengthy vendor procurement process, and other key decisions. However, several states emphasized the risks of moving forward in the absence of clear guidance, noting that if state decisions are not aligned with the federal expectations, the resulting rework would increase costs and potentially delay meeting important deadlines. Some states described the implementation deadline as unrealistic, noting that it increases the risk of errors that could lead to unnecessary coverage losses. In light of these risks, some states said early and clear guidance from CMS would be helpful, especially on issues such as the definition of medical frailty and other exemptions or the permissibility of self-attestation that could affect systems decisions.
A small number of states explicitly mentioned interest in the option for states to pursue good faith waivers to delay implementation of work requirements, noting that additional guidance would be needed to understand the criteria to obtain a “good faith waiver” and the state application process.
Figure 3
Several states reported workforce challenges, including the need to hire or reallocate staff in anticipation of increased workloads and the need for additional staff training. Many states reported that they will need to hire additional staff or reallocate existing staff to handle increased workloads from verifications, appeals, and enrollee outreach. States also anticipate the need for additional staff training, including training staff across departments and agencies (e.g., SNAP), to ensure eligibility workers understand the new rules and requirements, exemption criteria, and documentation requirements. A few states called out the additional workforce resources that will be necessary to conduct comprehensive and multi-modal outreach efforts and respond to the expected increase in enrollee inquiries.
A few states noted that staff are already managing major multiyear projects that are underway, such as eligibility system modernization projects, forcing staff and leadership to juggle competing demands. Similarly, limited staff capacity could cause spillover effects and result in less timely eligibility determinations for enrollees not subject to work requirements.
Even with implementation funds and federal matching payments for administrative costs, some states cited the increased costs of implementing work requirements as a concern. A number of states explicitly mentioned the fiscal implications tied to systems changes, hiring additional staff, and conducting outreach to enrollees. One state noted that, given the tight timeframe coupled with the enormity and complexity of the new requirements tied to system changes, interagency agreements, state rulemaking, and enrollee outreach, states may need to move forward on multiple parallel tracks, which could increase implementation costs and the risk for errors. Contracts for systems changes or new components are costly, and states noted that accelerated timelines often increase those costs. Some states also reported that the increased costs will further strain already constrained state budgets. In addition, some states discussed that new financial penalties for error rates in SNAP and Medicaid may potentially affect how they move forward with system changes. The new law provides $200 million in funding to states for systems development, with states able to access federal matching funds. The federal government generally provides 50 percent of the funds for administrative activities but pays for up to 90 percent of certain administrative costs, including for certain IT system changes.
While not asked directly about enrollee issues, several states cited concerns for applicants and enrollees, including anticipated confusion over the new requirements and possible coverage losses. States anticipate confusion among enrollees and applicants about the new work requirements and listed educating individuals among the challenges they will face. While states noted the importance of outreach to consumers, a few reported that efforts to move forward with communication and outreach without federal guidance could result in more enrollee confusion if CMS guidance does not align with state assumptions related to documentation requirements, exemption definitions, or data matching. Some states also expressed concern over possible coverage loss stemming from the accelerated implementation timeline and indicated that they plan to investigate ways they can minimize any coverage losses. One state noted particular concerns for enrollees in rural areas with limited internet access and those with jobs with fluctuating work hours.
Publisher: Source link