The 2025 reconciliation law could have major implications for nearly 15,000 federally certified nursing facilities and the more than 1.2 million people living in them. Nursing facilities provide medical and personal care services for older adults and people with disabilities. In 2023, Medicaid paid for 44% of long-term institutional care costs; 37% of long-term institutional care costs were paid for out-of-pocket; and the remaining 18% was covered by other public and private payers. Although provisions in the reconciliation law do not directly limit or reduce nursing facility services, changes to the Medicaid program could result in reduced payments from Medicaid for nursing facility care and may result in fewer people having Medicaid coverage of nursing facility care (see Box 1 for more on the 2025 reconciliation law.)
This data note discusses the impact of the 2025 reconciliation law on nursing facilities and examines the characteristics of nursing facilities and the people living in them with data from Nursing Home Compare, a publicly available dataset that provides a snapshot of information on quality of care in each nursing facility, and CASPER (Certification and Survey Provider Enhanced Reports), a dataset that includes detailed metrics collected by surveyors during nursing facility inspections. State-level data are also available on State Health Facts, KFF’s data repository with downloadable health indicators. Key takeaways from July 2025 data include:
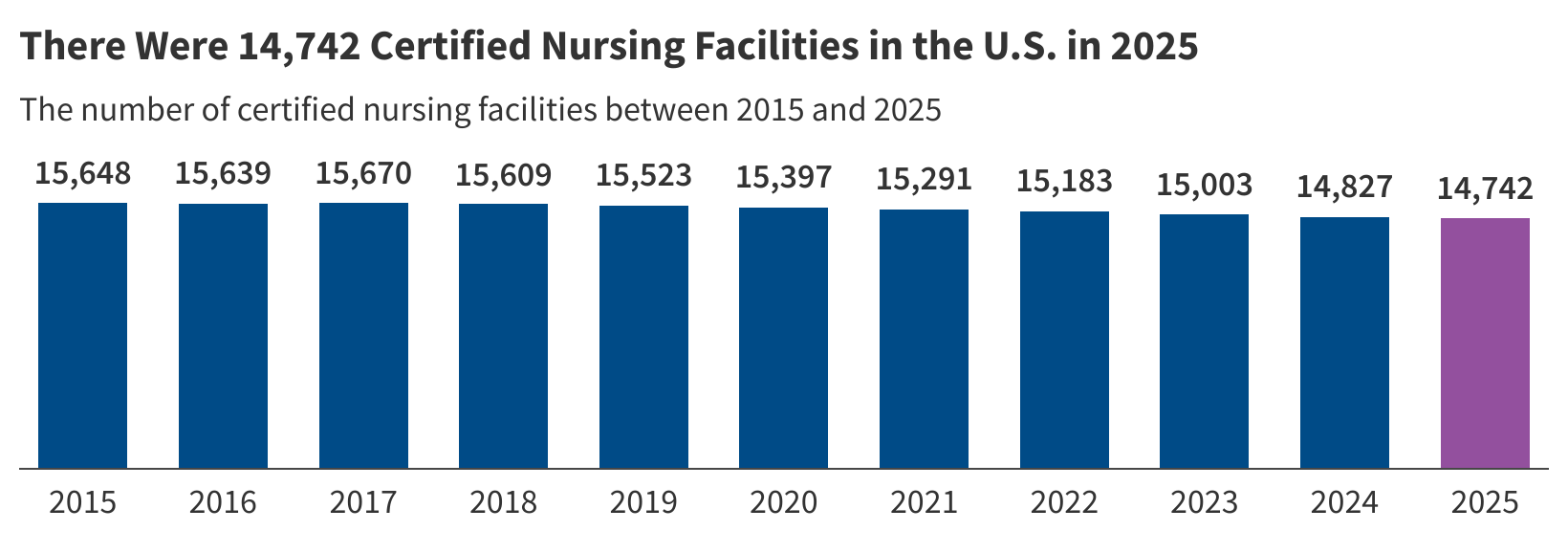
- There are 14,742 nursing facilities certified by CMS and about 1.24 million residents living in these certified nursing facilities (Figure 1).
- Nursing facility residents receive, on average, about 3.85 hours of nursing care per day from licensed practical nurses (LPN/LVN), registered nurses (RNs), and nurse aides (Figure 2).
- On average, nursing facilities receive 9.5 deficiencies over the course of a survey cycle (Figure 3).
- While nearly all facilities receive at least one deficiency over the course of a survey cycle, 27% of facilities receive serious deficiencies for actual harm or jeopardy posed to a resident (Figure 3).
Box 1: Major Provisions in 2025 Reconciliation Law that Could Impact Nursing Facilities
The reconciliation law, passed on July 4, 2025, includes significant health care policy changes, including some major changes could have implications for nursing facilities.
Broader federal spending cuts: The 2025 reconciliation law is expected to reduce federal Medicaid spending by $911 billion over the next decade, which could have implications for nursing facilities. Those spending cuts are likely to leave states with difficult choices about how to respond to reduced federal support including spending on long-term care which accounts for more than one-third of all Medicaid spending. States’ options for reducing spending on nursing facility care could involve reducing payment rates or restricting eligibility so that fewer people receive services.
State-directed payments (SDPs): SDPs require managed care organizations to make certain types of payments to health care providers, generally aimed at increasing provider payment rates to increase access to or quality of care. The reconciliation law reduced the maximum payment rate in SDPs from commercial rates to Medicare rates in states that have adopted the ACA expansion and to 110% of Medicare rates in non-expansion states. As a result of these changes, states may reduce payments to nursing facilities to comply with the caps in the new law.
Moratorium on eligibility rules: The reconciliation law delays implementation of two eligibility rules that would have increased Medicaid enrollment, especially among Medicare beneficiaries (dual-eligible individuals), a group that disproportionately uses nursing facility services, until 2034. CBO estimated that delaying these rules could reduce the number of dual-eligible individuals by around 1 million.
Reduced retroactive coverage period: The law reduces the period for which states must provide Medicaid coverage for qualified medical expenses from 90 days prior to the date of application for coverage to 60 days among non-expansion enrollees. Because entering a nursing facility is often a precipitating event for people to apply for Medicaid, this change may particularly affect Medicaid payments for nursing facilities.
Staffing rule: The law delays implementation of a Biden-era rule intended to help address long-standing concerns about staffing shortages and the quality of care in nursing homes until 2034. A Texas judge overturned key requirements from the rule in May 2025; and the Trump Administration rescinded the rule in December 2025.
Freezing home equity limit: The reconciliation law reduces maximum home equity limits on the homes of Medicaid nursing facility applicants to $1 million, starting in 2028. The limits will not grow over time and thus, become more binding in future years (as of 2025, 11 states had home equity limits higher than $1 million). Once this cap takes effect, people in those states who would otherwise be eligible may no longer qualify for Medicaid long-term care.
Immigration enforcement: The law provides additional funding to Immigration and Customs Enforcement to expand detention and deportation operations of immigrants in the U.S., raising questions about workforce shortages. Immigrants made up 21% of workers in nursing facilities in 2023.
Effective prohibition on new provider taxes or increases to existing ones: States are permitted to finance the non-federal share of Medicaid spending through healthcare-related taxes or “provider taxes” and often use those tax revenues to bolster provider payment rates. All but six states have taxes on nursing facilities. The law effectively prohibits states from enacting any new provider taxes or from increasing existing ones. Historically, states have used provider tax revenues as a mechanism to sustain Medicaid spending during budget shortfalls and to bolster payment rates, and the prohibition will reduce states’ ability to do so in the future. Recent data from a 50-state survey of state Medicaid programs show that 7 states (CO, KY, MA, MN, NJ, NC, and OK) planned to increase taxes on nursing facilities in FY 2026, though the new reconciliation law may prevent these increases from taking effect.
As of July 2025, there are 14,742 nursing facilities certified by CMS (Figure 1). The number of nursing facilities certified by CMS decreased by 6% between July 2015 and July 2025. There has generally been a steady decline during that time period. In order to receive payment under the Medicare and/or Medicaid programs, nursing facilities are required to follow certain regulations and be certified by CMS. The decreased number of nursing facilities reflects the net change in the number of certified facilities after accounting for newly-certified facilities and facilities that are no longer certified, including facilities that closed.
There are about 1.24 million residents living in certified nursing facilities (Figure 1). Since 2021, the number of nursing facility residents has gradually increased from 1.10 million to 1.24 million. However, between 2015 and 2025, the number of residents living in nursing facilities decreased by 9%, with most of that coming from a steep decline between 2020 and 2021, reflecting the effects of the COVID-19 pandemic. Prior to the pandemic, the number of residents was relatively steady, although it declined from 1.37 million in 2015 to 1.32 million in 2020. COVID-19 exacerbated the decrease in nursing facility residents—in part because nursing facility residents and staff incurred so many deaths during the pandemic.
Residents receive an average of 3.85 hours of nursing care per day, including 0.87 hours of LPN care, 0.68 hours of RN care, and 2.3 hours of nurse aide care (Figure 2). While staffing levels have gradually slightly increased overtime since 2022, the average hours of nursing care that nursing facility residents received declined by 7%, from 4.13 hours to 3.85 hours per resident each day, between July 2015 and July 2025. The decrease was driven by a 19% decline in registered nurse (RN) hours and a 7% decline in nurse aide hours. Licensed practical nurse (LPN) hours increased by 5% in this same time period. The 2024 rule would have required nursing facilities to meet minimum standards in staff hours for RNs and nurse aides but did not include any requirements for LPNs. A Texas judge overturned key elements of the rule in April 2025, the 2025 reconciliation law delayed all provisions of the rule until October 2034 (Box 1), and the Trump Administration rescinded the rule in December 2025. Previous KFF analysis show that just 19% of nursing facilities met the standards at the time of the rule’s passing.
The total hours of nursing care per resident decreased between 2015 and 2025, but rose briefly in 2021. The relatively higher staffing hours per resident in 2021 reflected the fact that the number of residents declined more quickly than the number of total nursing staff hours did between 2020 and 2021. In 2021, the number of staffing hours was 12% lower than in 2020 (data not shown). These lower staffing levels in the last several years align with data as of March 2024 showing that the number of workers employed at long-term care facilities continues to remain below pre-pandemic levels.
Box 2: Direct Care Staff in Nursing Facilities
Registered Nurse (RN): Registered nurses (RNs) are responsible for the overall delivery of care to the residents and assess needs of nursing facility residents. RNs are typically required to have between two and six years of education.
Licensed Practical Nurse (LPN) and Licensed Vocational Nurse (LVN): LPNs/LVNs provide care under the direction of an RN. Together, RNs and LPNs/LVNs make sure each resident’s plan of care is being followed and their needs are being met. LPNs/LVNs typically have one year of training.
Certified Nurse Aides/Assistants (CNAs): CNAs work under the direction of a licensed nurse to assist residents with activities of daily living such as eating, bathing, dressing, assisting with walking/exercise, and using the bathroom. All CNAs must have completed a nurse aide training and competency evaluation program within 4 months of their employment. They must also pursue continuing education each year.
Nursing facilities receive an average of 9.5 deficiencies over the course of a survey cycle and 27% of facilities receive deficiencies for actual harm or jeopardy (Figure 3, Box 3). While nearly all facilities receive at least one deficiency during a survey cycle, this analysis focuses on the share with serious deficiencies since there is wide variation in the types of deficiencies a facility may receive. Both the average number of deficiencies and the share of facilities with serious deficiencies have increased over time, which could reflect increased oversight and low staffing levels that lead to staffing-related deficiencies. Between 2015 and 2025, the average count of deficiencies per nursing facility increased from 6.8 to 9.5, an increase of 40%. The increase was generally steady overtime, except for two stable periods: 1) between 2020 and 2022 and 2) between 2024 and 2025 (though 2024 and 2025 reported the highest number deficiencies during the 10-year period). The share of facilities reporting serious deficiencies between 2015 and 2025 increased from 17% to 27%, with a slight decrease between 2024 and 2025. A 2023 report on nursing home staffing by Abt Associates found that better-staffed nursing homes are typically cited for fewer deficiencies or violations of federal regulations, suggesting there may be a relationship between the increase in deficiencies and the general decrease in staffing levels over the 10-year time period.
Box 3: Deficiencies in Nursing Facilities
Nursing facilities receive deficiencies when they fail to meet the requirements necessary to receive federal funding. Deficiencies are often given for problems which may have negative effects on the health and safety of residents. Commonly cited deficiencies include a failure to provide necessary care, failure to report abuse or neglect, and violation of infection control requirements. Each of these categories has specific regulations that state surveyors review to determine whether facilities have met the standards.
Deficiencies are characterized by their level of severity: Deficiencies for “actual harm” or “immediate jeopardy” are the most severe and are grouped together under the term, “serious deficiencies.” CMS defines “actual harm” as a “deficiency that results in a negative outcome that has negatively affected the resident’s ability to achieve the individual’s highest functional status.” “Immediate jeopardy” is defined as a deficiency that “has caused (or is likely to cause) serious injury, harm, impairment, or death to a resident receiving care in the nursing facility.” These can include citations to facilities for physically abusing residents, failure to maintain safe living quarters, or failure to provide CPR or other basic life support when necessary for residents.
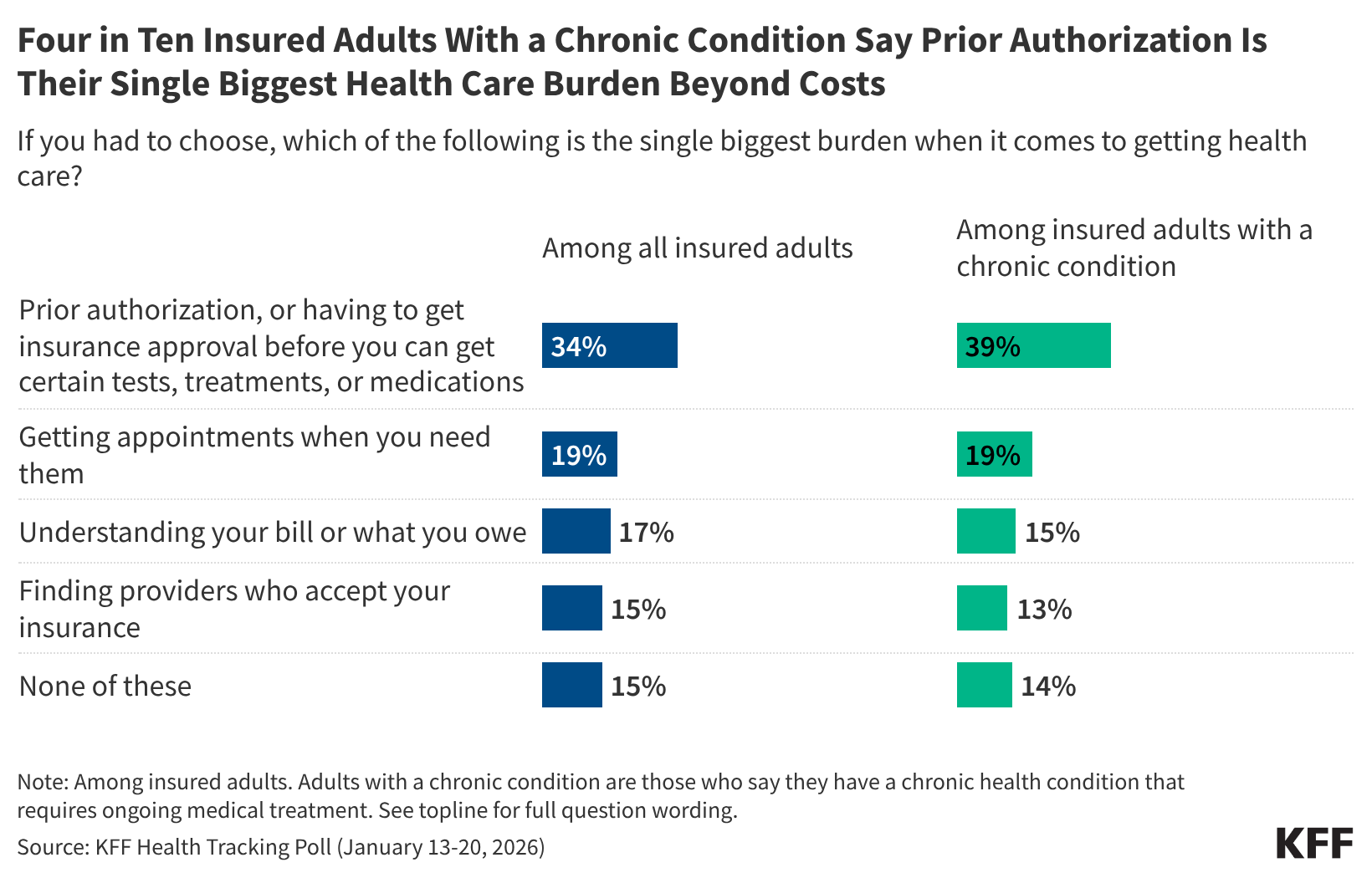
Medicaid is the primary payer for 63% of nursing facility residents; Medicare for 14% of residents; and the remaining 23% of residents have another primary payer (ex. out-of-pocket) (Figure 4). The share of residents by primary payer has stayed relatively stable over time. Medicare does not generally cover long-term care but does cover up to 100 days of skilled nursing facility care following a qualifying hospital stay. KFF polling shows that four in ten adults overall incorrectly believe that Medicare is the primary source of insurance coverage for low-income people who need nursing facility care.
Nearly three-quarters (73%) of nursing facilities are for-profit, one-fifth (20%) are non-profit, and the remaining seven percent are government-owned (Figure 5). The share of facilities by ownership type has also stayed relatively stable over time but there was increasing scrutiny over the 73% of facilities that are for-profit during the prior Administration. Despite little change in the type of ownership, there have been reports of private equity firms purchasing nursing facilities and changing operations to increase profits, resulting in lower-quality care. The GAO estimates that about 5% of nursing facilities had private equity ownership in 2022.
The Biden Administration issued a final rule in November 2023 on nursing facilities (separate from the April 2024 staffing rule that was delayed by the 2025 reconciliation law and then rescinded by the Trump Administration in December 2025). The 2023 nursing facility rule requires nursing homes enrolled in Medicare or Medicaid to disclose detailed information regarding their owners, operators, and management, including:
- Anyone who exercises any financial control over the facility;
- Anyone who leases or subleases property to the facility, including anyone who owns 5% or more of the total value of the property; and
- Anyone who provides administrative services, clinical consulting services, accounting or financial services, policies or procedures on operations, or cash management services for the facilities.
Facilities must also disclose whether any of the owning or managing entities are a private equity company or real estate investment trust (REIT). Facilities began self-reporting this data to CMS in early 2024 and the data is now available to the public. However, these data may be incomplete for now as fewer than 100 facilities report private equity ownership and just over 300 facilities report REIT ownership. Other research estimates those counts to be higher.
This work was supported in part by The John A. Hartford Foundation. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
Publisher: Source link