The pandemic-era continuous enrollment provision sustained Medicaid for millions of enrollees, making it easier for children to get on and stay on coverage. Between February 2020 and April 2023 with continuous enrollment in place, child enrollment in Medicaid and CHIP increased by 20%. While national child enrollment has since nearly returned to pre-pandemic levels, state child eligibility expansions may help to bolster coverage in the aftermath of the unwinding of the continuous enrollment provision.
During the pandemic, states took advantage of a range of flexibilities to facilitate access to Medicaid and CHIP coverage, such as eliminating or waiving premiums for Medicaid and CHIP. Following the end of continuous enrollment, recent federal policies have sought to extend coverage protections for children. The Consolidated Appropriations Act, 2023, required all states to implement 12-month continuous eligibility for children beginning on January 1, 2024. Expanding on that continuous eligibility policy to provide more stable coverage over a longer period of time for vulnerable populations, the Centers for Medicare and Medicaid Services (CMS) has encouraged states to seek approval to provide multi-year continuous eligibility for children through Section 1115 demonstration authority. CMS also published an Eligibility and Enrollment final rule earlier this year that eliminates lock-out periods for failure to pay premiums in CHIP and requires smoother transitions between Medicaid and separate CHIP programs, among other changes.
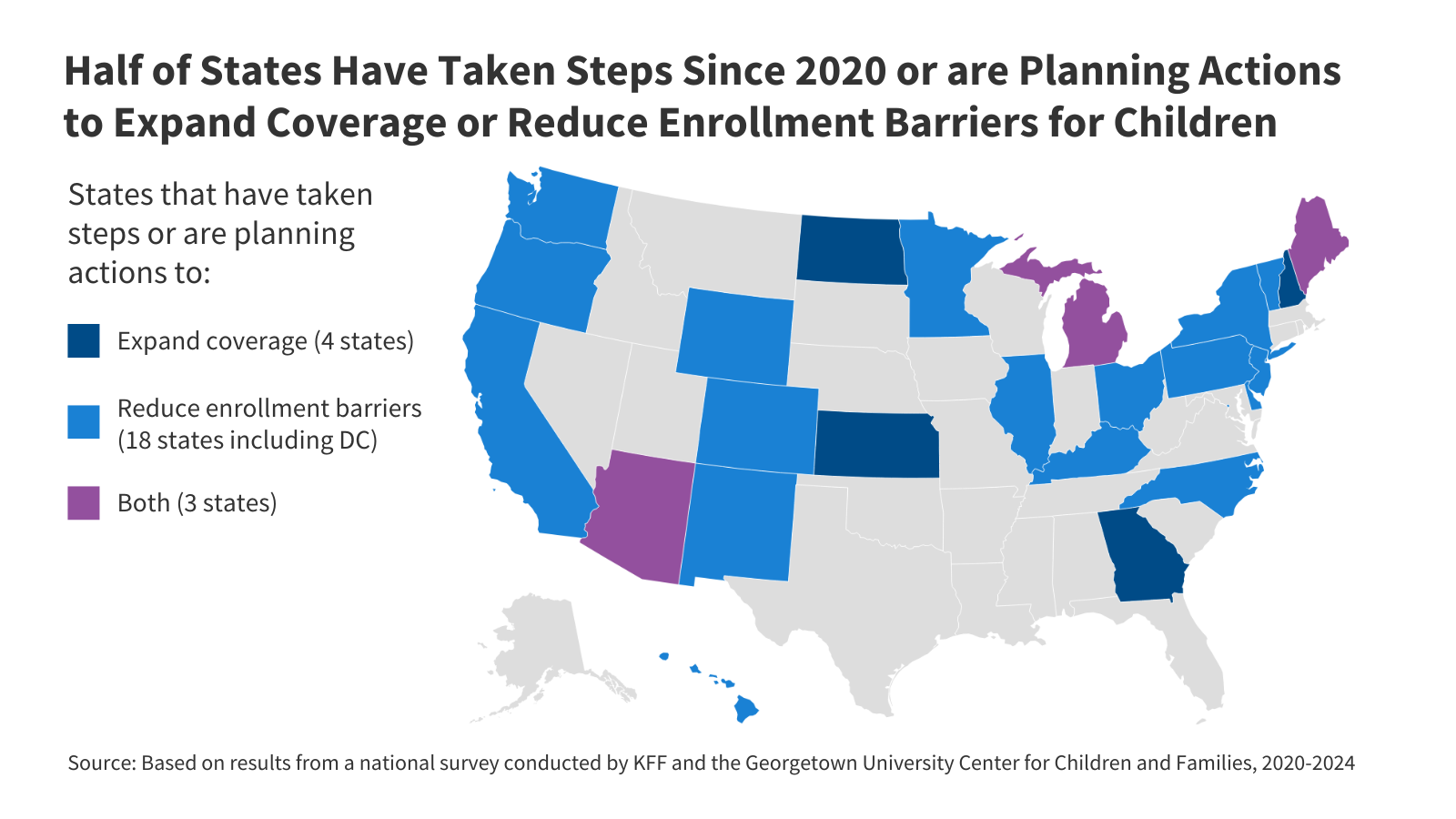
This policy watch identifies states that have expanded access to Medicaid and CHIP coverage for children or have adopted policies to make it easier for children to maintain coverage since the start of the pandemic. Data are from annual surveys of state Medicaid and CHIP program officials conducted by KFF and the Georgetown University Center for Children and Families.
Facilitating Medicaid/CHIP Coverage for Children
Building on the experience with continuous enrollment and other pandemic-era protections, since 2020 half of states (25) have taken steps or are planning actions to expand coverage or reduce enrollment barriers for children (Figure 1). Four states expanded coverage by increasing child income eligibility for Medicaid and CHIP and/or adopting the federal option to cover lawfully-residing immigrant children without the 5-year wait. Eighteen states have taken steps or are planning actions to reduce enrollment barriers for children, such as by pursuing multi-year continuous eligibility waivers for young children, eliminating or continuing to suspend premiums, or transitioning from a separate CHIP program to a CHIP-funded Medicaid expansion program. Three states have taken steps to both expand coverage and reduce enrollment barriers.
Expanding Coverage
Four states recently expanded coverage by increasing income eligibility levels for children in Medicaid and CHIP (Figure 2). In 2022 the Kansas legislature increased CHIP eligibility to 255% of the federal poverty level (FPL). In the past year, Arizona increased eligibility from 205% FPL to 230% FPL in its separate CHIP program, Maine raised Medicaid child eligibility from 213% FPL to 305% FPL, and North Dakota expanded Medicaid child eligibility to 205% FPL, up from 175% FPL. With these changes, Idaho is the only state with a child eligibility level below 200% FPL. Across all states, the median children’s upper eligibility level is 255% of the Federal Poverty Level (FPL) ($65,841 for a family of three in 2024). Twenty states now cover children at or above 300% FPL.
Since 2020, three states have newly taken up the federal option to cover lawfully residing immigrant children without the 5-year wait. Most lawfully residing immigrants must wait five years after they obtain qualified status before they can enroll in Medicaid or CHIP. However, states have the option to waive the five-year waiting period for lawfully residing children, otherwise known as the Immigrant Children’s Health Improvement Act (ICHIA) option. Georgia, Michigan, and New Hampshire recently adopted this option, joining 34 other states and the District of Columbia that adopted prior to 2020 (Figure 3). Indiana plans to eliminate the waiting period for children and pregnant individuals in 2025.
Six states (Connecticut, Maine, New Jersey, Rhode Island, Utah, and Vermont) newly provide fully-state funded coverage to all income-eligible children regardless of immigration status since 2020. These programs extend coverage to immigrant children who are ineligible for federally funded coverage because they do not have qualified status or because they are undocumented. Connecticut only covers children under age 13 and Utah caps the number of children who can be enrolled. Six states (California, Illinois, Massachusetts, New York, Oregon, Washington) and the District of Columbia began providing comprehensive state-funded coverage for children regardless of immigration status prior to the COVID-19 public health emergency. By 2025, Colorado and Minnesota plan to offer state-funded Medicaid-like coverage to income-eligible children regardless of immigration status.
Reducing Enrollment Barriers
Thirteen states have federal approval or are in the process of developing waivers to expand upon the 12-month continuous eligibility requirement and implement multi-year continuous eligibility for young children. Continuous eligibility has been shown to reduce Medicaid disenrollment and “churn” rates (rates of individuals temporarily losing Medicaid coverage and then re-enrolling within a short period of time). When individuals churn on and off coverage, the gaps in coverage may limit access to care or lead to delays in getting needed care, which can be especially problematic for young children who receive frequent screenings and check-ups. In September 2022, CMS approved Oregon’s waiver to implement continuous eligibility for children from birth to age six as well as 24 months of continuous eligibility for nearly all enrollees ages six and older. Since then, CMS has approved multi-year continuous eligibility requests for children in Washington and New Mexico. Six states have submitted section 1115 waivers and four states are in the process of developing waivers to implement multi-year continuous eligibility for young children (Table 1).
Twelve states have eliminated Medicaid or CHIP premiums since 2020 or continue to suspend premiums, reducing financial barriers to coverage for children. While new rules related to 12-month continuous eligibility prohibit states from disenrolling children because of failure to pay premiums during the continuous eligibility period, premiums can still act as a barrier to enrollment because states can require families to pay the initial premium before they can enroll their child. During the COVID-19 public health emergency, most states that charged premiums suspended or waived them for some or all enrollees. Nine states — California, Colorado, Illinois, Maine, Maryland, Michigan, New Jersey, North Carolina, and Utah — have eliminated Medicaid and/or CHIP premiums since 2020. Utah eliminated CHIP premiums in July but increased other cost-sharing requirements at the same time (Figure 4). In three states that charged premiums prior to the pandemic (Arizona, Delaware, and Vermont), premiums remain suspended. Delaware is awaiting CMS approval to discontinue premiums entirely and Vermont has suspended premiums indefinitely. A total of 18 other states still charge premiums. Twenty states and the District of Columbia did not charge premiums or enrollment fees prior to 2020.
Since 2020, a total of five states (Illinois, Maine, North Carolina, Kentucky, and Wyoming) have transitioned all child enrollees from the state’s separate CHIP program to a CHIP-funded Medicaid expansion program. Rules governing administration of and eligibility processing in separate CHIP programs differ from Medicaid. Sixteen additional states choose to cover all uninsured children eligible for CHIP in Medicaid (known as M-CHIP), but states can also choose to cover uninsured children eligible for CHIP through a separate CHIP program only (2 states) or through a combination of a separate CHIP and M-CHIP (28 states) (Figure 5). Covering CHIP children in Medicaid streamlines administration and provides all children with child-focused EPSDT Medicaid benefits and other Medicaid protections, including limitations on cost-sharing, while operating a separate CHIP allows states to alter benefit packages and delivery systems and provides more flexibility to impose premiums and cost sharing. Covering CHIP children in Medicaid can also prevent children from losing coverage during necessary transitions between Medicaid and separate CHIP programs.
Publisher: Source link