This story was reported in partnership with Uncloseted Media, a nonpartisan, investigative, LGBTQ-focused news publication.
Twenty-year-old Dorian McCuller sat on his porch in Newport News, Virginia, trying to say “HIV” out loud. “It’s really scary. I feel like if I’m too open about it, people will use it as a target.”
Growing up in the South, McCuller felt a lot of stigma about being gay. When he was 13, he came out to his grandmother.
“She said if I am gay, ‘don’t have sex. A demon will crawl up [your] ass,’” McCuller said, adding that at the time he took that to mean he’d contract HIV. McCuller’s grandmother says she only remembers advising McCuller not to have sex because he was a virgin.
(Parker Michel-Boyce, independent photojournalist for Fierce Healthcare/Uncloseted Media )
Fast forward to last year, McCuller got the call that he was HIV positive a few days after his 19th birthday. Someone McCuller was intimate with told him they needed to talk. “I immediately knew it was in the realm of HIV,” he said. “I got tested a few days later.”
In the last 30 years, HIV rates have gone down, in large part because of the game-changing prescription drug pre-exposure prophylaxis (PrEP), which reduces the risk of contracting HIV through sex by 99%. Since the FDA approved the drug in 2012, more people have started to use it, and HIV rates have steadily decreased. But not everyone is seeing the same results.
From 2019 to 2022, 94% of white people who could benefit from PrEP were prescribed it, while only 13% of Black and 24% of Latino people were. HIV— which has claimed an estimated 42.3 million lives to date and remains a global public health issue—continues to have a disproportionate impact on people of color, men who have sex with men, and trans women. The lifetime risk of acquiring HIV is still 1 in 3 for Black gay and bisexual men, according to data from the Centers for Disease Control and Prevention (CDC).
Ending the HIV epidemic hinges on both treatment and prevention, particularly through access to PrEP. For at-risk individuals living in the U.S. South—where HIV is a daunting reality—PrEP use is very low compared to the number of new HIV cases.
If I had known, I would have gotten on PrEP.
Dorian McCuller, 20, Virginia
The South had 53% of new HIV diagnoses in 2022 but represented only 39% of PrEP users in 2023. Regionally, Black people made up 48% of new HIV diagnoses in 2022, but only 22% of PrEP users in 2023. While PrEP is more accessible in metropolitan areas, educational barriers, healthcare costs and anti-LGBTQ+ stigma still hinder access, particularly in rural areas and the Bible Belt.
(Parker Michel-Boyce, independent photojournalist for Fierce Healthcare/Uncloseted Media )
“It felt like a slap in the face,” said McCuller, who is still processing the diagnosis from last year. “It made me a lot more self-conscious, like as far as self-worth…I just find myself questioning a lot of myself, and it didn’t really start until I became positive.”
“If I had known, I would have gotten on PrEP,” he said, adding that he had never heard of the drug until after he contracted the virus.
McCuller is far from alone in having lacked awareness about PrEP. Gina Bailey Herring, an advanced practice registered nurse and a research nurse practitioner at Emory University, has seen a large number of late adolescents with new HIV diagnoses. “That is telling us that they’re not being offered PrEP services in their pediatrician’s office,” she said. “There are many zip codes in the U.S. where only infectious disease providers are providing PrEP.”
Chris Bean, a 39-year-old in Kissimmee, Florida, had told his doctor—-who he had been seeing for three years—-that he was gay, in an open relationship and having unprotected sex with his partner and other men.
“She never once mentioned PrEP,” Bean told Fierce Healthcare/Uncloseted Media.
Two years later, in 2022, Bean contracted HIV. “I was completely numb when I found out,” he said. “I just completely glazed over when I got the call. It took me a year to process it.”
Moving HIV ‘from the moral arena to the medical arena’
Stigma toward the LGBTQ+ community is rampant in the U.S. The American Civil Liberties Union is currently tracking 530 anti-LGBTQ+ bills in the U.S., many of them in the South. Conservatives have called on ending what they refer to as “left-wing gender insanity” and have referred to trans and queer people as “filth.” Anti-LGBTQ+ threats and vandalism has been reported in at least 10 states since June 2024, including bomb threats and burned Pride flags.
In some southern states, even PrEP is under attack. A highly watched case in Texas, brought by a group of individuals and Christian-owned businesses, resulted this summer in a ruling by the U.S. Court of Appeals for the 5th Circuit that they cannot be forced to provide PrEP for free. The plaintiffs argued that requiring PrEP violates the Religious Freedom Restoration Act, stating that it “encourage[s] and facilitate[s] homosexual behavior,” which conflicts with their religious beliefs. While the case still hangs in the balance, hundreds of preventive benefits remain at stake for more than 150 million privately insured Americans, including the most vulnerable populations.
Anti-LGBTQ+ stigma, which can come from religious‐based negative attitudes, may have unintended consequences when it comes to PrEP access for the most vulnerable.
(Kate Medley for Fierce Healthcare/Uncloseted Media)
“In the Black Church, the queer community is not discussed,” said Natalie Farrior, a Black trans woman from rural North Carolina, whose father was a pastor. She said religion impacted how she related to her sexuality.
Farrior, who contracted HIV a few years ago, is still religious, but said she doesn’t feel accepted at her church, so has spots around town where she prays in private.
(Kate Medley for Fierce Healthcare/Uncloseted Media)
“If you are expected of being [a] homosexual, you are immediately prayed for,” said Farrior, 29, who came out as a gay man before coming out as trans later in adulthood.
“We have a long way to go, specifically in the south where our faith or religious beliefs are dictating policy,” said Leisha Mckinley-Beach, a national HIV expert and founder and CEO of training institute Black Public Health Academy. “They are dictating health outcomes. That means faith carries a lot of weight in a region like the South.”
Mckinley-Beach says Christian providers may project their religious beliefs onto their patients. “I know of providers who have prioritized their religious beliefs,” she said. “When you have people in the LGBTQ population who have to overcome one more hurdle to get closer to PrEP, that’s exhausting.”
While religion may be fueling some medical bias when it comes to PrEP access, it still has a place to be life affirming, said Stacy Smallwood, Ph.D., executive director of Wake Forest University School of Divinity’s Faith Compass Center.
“A lot of the work that we do is telling a different story, changing the narrative, because so much of the work that has been put in front of us, so much of the history, has been around stigma,” Smallwood said. “Even though we have 2024 tools to address HIV prevention and treatment, there are still 1980s and 1990s mindsets that have not come along with the technology and the innovation.”
Then they’re going to start treating you differently immediately. You’ll hear the tone change in their voice because you’re gay.
Sloan Parker, 28, Alabama
Historical stereotypes feed into an untrue, moralistic stance that people affected by HIV are to blame, he added. “We engage in this victim blaming, that your vulnerability is the result of you not making good choices.”
Sloan Parker, a 28-year-old gay man from “a four-way stop of a town” known as Ford City, Alabama, couldn’t risk the medication showing up on his parent’s insurance: “I knew about PrEP forever. But I was just a college student and getting over my internalized homophobia. I was freshly out as gay, and I couldn’t risk [my parents] seeing it.”
(Sloan Parker)
Parker didn’t feel comfortable calling urgent care to talk about PrEP because of the medical bias he felt in the South. “The first question is, why are you having sex?” he said. “Then they’re going to start treating you differently immediately. You’ll hear the tone change in their voice because you’re gay.”
Being queer in the South is not talked about. It’s shunned.
Natalie Farrior, 29, North Carolina
These experiences turn marginalized people away from further engaging with the healthcare system. LGBTQ+ adults trust their providers 30% less than cisgender, heterosexual people, a 2023 survey found. Nearly a third of LGBTQ+ people felt dismissed by their doctor and were also 26% more likely to delay, avoid or skip a health screening than cisgender, heterosexual people.
“When we’re talking about communities that maybe have a lot of medical mistrust, we need to come up with innovative ways to bring that prescriber to a place where someone actually feels more comfortable accessing services,” Jeremiah Johnson, executive director of Prep4All, said. “There’s no reason that a homeless shelter or an LGBTQ center can’t be turned into a proper access point.”
(Kate Medley for Fierce Healthcare/Uncloseted Media)
“For my community, we are invisible in most spaces,” said Farrior, who grew up in a town of 950 people in North Carolina. “It boils down to the Southern mindset and mentality. Being queer in the South is not talked about. It’s shunned. You have a lot of these men that are living double lives. They’re putting themselves at risk and everyone else at risk and it’s scary.”
Right now, that PrEP bottle is like you setting the rainbow flag out on the counter mentally. It’s something explicitly gay.
Sloan Parker, 28, Alabama
On Grindr, a dating and hookup app for the queer community, Uncloseted Media/Fierce Healthcare reached out to men in the Tupelo, Oklahoma, area to see who had heard of PrEP. Eleven of 21 men had heard of it but never considered using it. Five had never heard of it. Only five were on it.
Marketing can inadvertently contribute to stereotypes about who should or should not be on PrEP. Parker noted the ads he has seen are geared toward an audience of gay men. But anyone can contract HIV, regardless of sexual orientation or gender identity.
“You have to market it as specifically not a gay thing,” Parker said. “So straight people can also go to their doctor and say they’re sexually active and want to be on PrEP and then go do it. Right now, that PrEP bottle is like you setting the rainbow flag out on the counter mentally. It’s something explicitly gay.”
Local, grassroot efforts to reach at-risk patients
Doctors may not be prescribing PrEP because they don’t know which patients are at risk because they aren’t asking. Less than 40% of providers conduct sexual histories with patients, according to one estimate. A separate survey found only half routinely ask their patients about their sexual orientation. Of those who do not ask, more than 40% said that sexual orientation is irrelevant to care. Part of the issue is a lack of training: 44% of U.S. medical schools lack formal sexual health curricula, according to one estimate.
PrEP requires a prescription from an authorized provider like a doctor, nurse or in some states, a pharmacist. Though the overall number of providers offering PrEP is growing, from 2014 to 2019 the number of prescribing physicians dropped from 80% to 68%. Infectious disease doctors still prescribe the most of any specialty. Less than a third of PrEP providers practiced in the South.
“There are concerns, often from primary care physicians, that they are not infectious disease doctors so they don’t know how to do it,” Justin Smith, director of the Campaign to End AIDS, told Fierce Healthcare/Uncloseted Media. “What we have to try to do is say this is basic preventive healthcare, if you are a primary care provider, this is within your scope of practice.”
We need to move this from the moral arena to the medical arena: it’s just a disease. Everybody should have the right to medical treatment.
Kathie Hiers, CEO , AIDS Alabama
Black women in particular have been left behind in the fight against HIV. Less than 2% of eligible Black cisgender women take PrEP, according to one estimate. Black women make up 14% of the U.S. female population, but accounted for half of all new HIV diagnoses among women in 2022. That year, most infections among women were attributed to heterosexual contact.
To combat misperceptions, one clinic in Mobile, Alabama, has staffed cisgender and heterosexual women to help encourage Black women in the community to get on PrEP. Shell Health, run by AIDS Alabama South, works with local sorority and fraternity chapters to fundraise and host STI/HIV testing events. Students who get tested can then sign up for PrEP.
“We’ve made a concerted effort to get as many of those women into the clinic as we can,” Kathie Hiers, CEO of AIDS Alabama, said. “If we can get folks that look like the people we’re trying to serve, you’re going to have better success.”
(AIDS Alabama)
Candace Taylor, executive director of AIDS Alabama South, understands the stigma that many Black women face. “We are raised: ‘You don’t have sex unless you get married, you go to church, you’re not supposed to do this,’” she said.
To help educate the community, the organization hosts a free quarterly event called Girls Who Know with a round table discussion on women’s health, including HIV and AIDS. “We need to move this from the moral arena to the medical arena: it’s just a disease. Everybody should have the right to medical treatment,” Hiers said.
AIDS Alabama South has a presence at a rotating community health fair in local middle schools each year. It also offers a TeenTalk program focused on HIV and STI prevention at a local high school, and works with the Alabama Department of Public Health and rural county clinics. It advertises on billboards, in radio ads and with local businesses. “We call it ‘bar outreach’…we have posters in local restaurants and bars that have a QR code,” Taylor said. Certain policies complicate school efforts. “We’re an opt-in state, where parents have to give permission for us to talk to their students [about sexual health],” Taylor said.
(AIDS Alabama South)
“They didn’t cover gay sex in sex ed,” McCuller told Fierce Healthcare/Uncloseted Media. “I didn’t learn about HIV or PrEP. Now that I’m thinking about it, it’s ridiculous. A lot of stuff I should have known before I got to this point.”
In addition to education, reaching people in remote areas— or so-called PrEP deserts—is critical. A desert is defined as an area where a PrEP provider couldn’t be accessed within a 30-minute drive. A 2019 study found that regions in the South are nearly eight times more likely to be classified as PrEP deserts than the Northeast.
In Alabama, for example, Taylor said some patients have to travel two hours to get to Mobile County for services. That’s why the Shell clinic staff drive a van around the state and offer PrEP and HIV testing, sometimes going straight to people’s homes.
“We try to make it where they don’t have to travel so far and we want to meet them in their environment, meet them in their communities,” Taylor said.
That’s how I became HIV positive. Because the access went away.
Sloan Parker, 28, Alabama
As co-founder of what was reported as the first LGBTQ+ clinic in Mississippi, Leandro Mena, M.D., healthcare consultant at All-In Health Solutions and former director of the CDC Division of STD Prevention, knows how much social determinants like reliable transportation can affect access. “We have people coming from all over the state to that single clinic,” he said, referring to the clinic he helped found. Patients might not be the best at anticipating their own challenges, he added: a patient who missed an appointment said they were relying on a friend for a ride, but they never showed up. More than one million households, mostly in rural counties, do not have access to a car.
(Leandro Mena)
When living in Atlanta, Parker never had an issue with exposure to HIV because so many people were taking precautions. After moving back to Ford City, Alabama, however, he searched for the nearest access point for PrEP. “Nashville popped up, which is 110 miles away. And then Birmingham is another 105 miles away. And since it was COVID times, I wasn’t really going anywhere.”
“That’s how I became HIV positive. Because the access went away,” Parker said.
Red tape, insurer non-compliance and costs keep PrEP out of reach
Natalie Farrior had known about PrEP since coming out at 14. She got on the medication as soon as she could at 18 through a Blue Cross insurance plan her university provided. After taking the medication for six years, her insurance coverage ended at 24 when she graduated, and she couldn’t afford to pay for it. What cost $80 for a month’s supply on her insurance skyrocketed to $500 for the same bottle.
“I was off of PrEP for a maximum of three months. I would have started my new job and had access soon [through new insurance], but by then I was HIV positive,” she says. “I had a whole mental breakdown when I found out. It took a lot of screaming and crying it out. I did everything you were told to do to avoid this and it still happened.”
(Kate Medley for Fierce Healthcare/Uncloseted Media)
“I think for folks who don’t have health insurance, the options are more limited, especially based on where you live,” Smith of the Campaign to End AIDS said. Community-based organizations specializing in HIV may have programs to support uninsured patients, Smith added, but people might not know they exist. “I don’t think we’ve done a good job [in public health] of fully communicating that.”
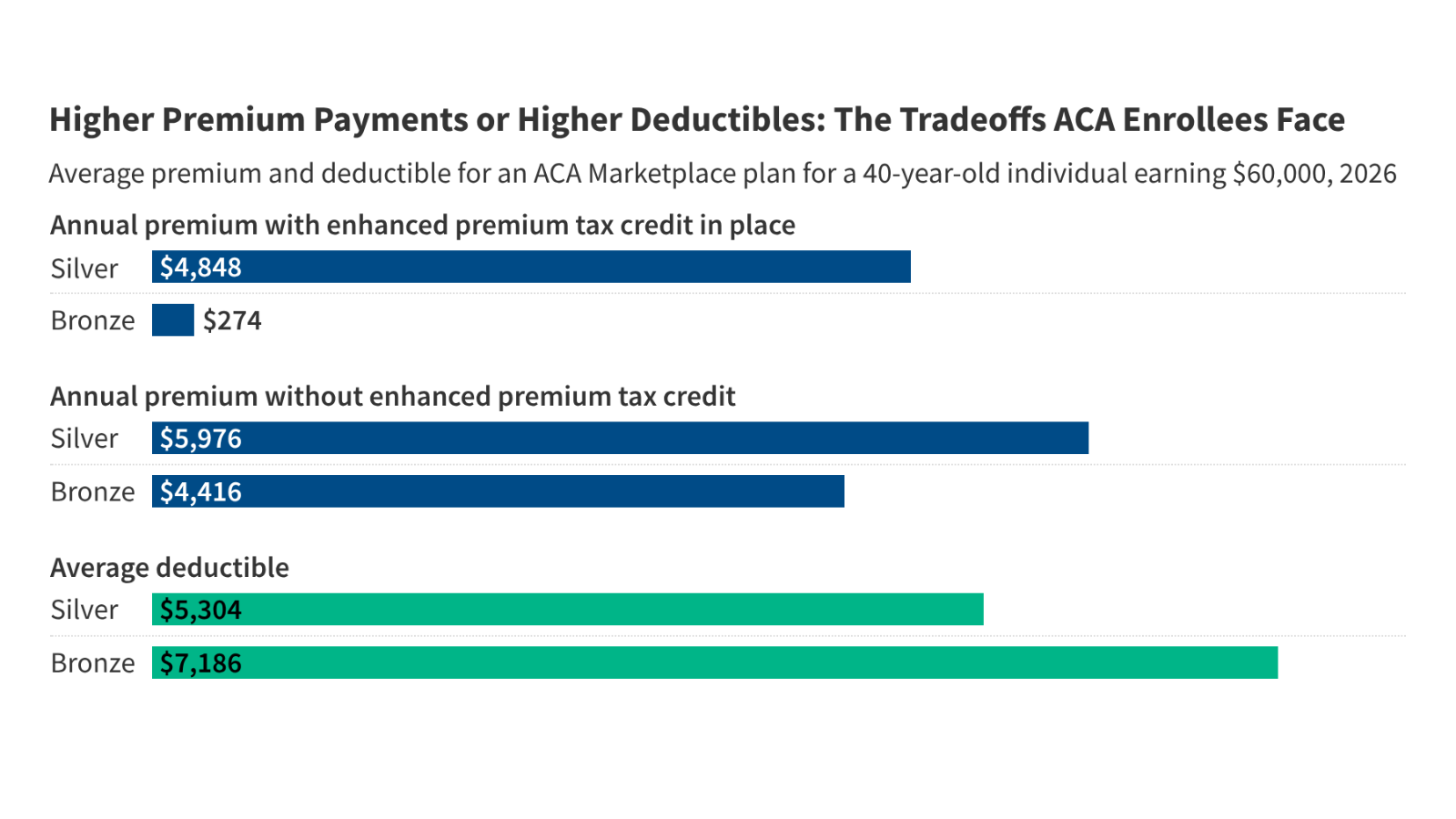
The Affordable Care Act (ACA) requires many plans to cover certain recommendations made by the U.S. Preventive Services Task Force, an independent volunteer advisory board of medical experts. In 2021, the Task Force put out a “grade A” recommendation that private and Medicaid expansion plans cover PrEP with no cost-sharing to patients. It also mandated these plans to cover PrEP-related doctor’s visits and labs at no charge. “Under the Affordable Care Act, PrEP is free under almost all health insurance plans,” according to HIV.gov.
Despite the mandate, patients still face prior authorizations, which can cause delays in treatment, or even bills for co-pays. Up to a third of commercially insured PrEP users paid out-of-pocket for lab testing after the 2021 mandate, a CDC study found. “These findings shed light on the scope of ACA mandate noncompliance by commercial payers,” the study concluded.
It is out of control. We need enforcement.
Carl Schmid, Executive Director , HIV+Hepatitis Policy Institute
While plans are allowed to use tactics to determine some coverage limitations, they must make medical necessity exceptions and may only use such techniques when the guidance is not already specific. It is not unexpected for a plan to limit the number of times a service, like bloodwork, can be done per year. But USPSTF’s recommendation on PrEP defers to CDC guidelines that clearly lay out how often such services are needed.
“Health plans partner closely with providers to ensure patient access to PrEP and related preventive health services with no cost-sharing,” a spokesperson for America’s Health Insurance Plans, a trade group for health insurance companies, told Fierce Healthcare/Uncloseted Media.
The recourse for patients facing charges when these preventive services should be free is limited. They can either try to push back on their health plan, rely on their provider to do so or submit a complaint to agencies like a state attorney general’s office or the Division of Insurance.
“It is out of control,” Carl Schmid, executive director of HIV+Hepatitis Policy Institute, told Fierce Healthcare/Uncloseted Media. “We need enforcement.”
In a lengthy response, the Centers for Medicare and Medicaid Services (CMS) told Fierce Healthcare/Uncloseted Media that it takes enforcement of preventive services coverage seriously. Generally, states have authority over fully insured plans, a spokesperson said, while CMS enforces non-federal government plans. The Department of Labor oversees private employer group health plans. The Department of Labor declined to comment for the story.
CMS has gotten complaints about PrEP coverage. It investigates single complaints, or for complaints that point to a possible systemic issue, comprehensively reviews a plan’s operations and business practices in a market conduct exam. CMS recently closed three non-federal governmental plan investigations about coverage of PrEP, the agency spokesperson said.
In two of those investigations, the plans were found to be in violation of preventive service requirements, according to CMS. When a violation is identified, plans are required to conduct a self-audit to identify all other claims affected by the violation. Those claims were then required to be re-adjudicated, with refunds to patients. The plan also had to demonstrate they put changes in place to prevent it from happening in the future.
“CMS has authority to issue civil money penalties when a plan or issuer fails to make corrections for violations within 30 days of the date the plan or issuer knew or should have known of the violation,” the spokesperson said.
The agency is considering additional changes “to help address potentially high costs associated with PrEP services and to thereby reduce issuer incentives to restrict coverage and access to care,” the spokesperson said. It has proposed to incorporate PrEP as a new cost factor in HHS-operated risk adjustment models starting in 2026. This “would seek to address the unique risk of adverse selection to the extent that utilization of PrEP services differs between plans.”
Data points to regional disparities in coverage. One study found qualified health plans in the South, the region with the most annual new HIV infections, were nearly 16 times as likely to require prior authorization for PrEP in 2019 as those in the Midwest, West and Northeast. It is a practice that more Black and Hispanic than white Americans report experiencing.
Despite payer claims that they need a prior authorization to determine a patient’s risk, that is not their arena, Schmid says. “We don’t need an insurance company to determine if you’re at risk or not. That’s between the provider and the PrEP user.” Prior authorization is among the top-cited barriers to PrEP by clinicians.
Two of the manufacturers behind PrEP drugs, Gilead Sciences and ViiV Healthcare, offer programs to help patients afford the medications. But these programs do not help cover the costs of the doctor’s visits or labs that are required as part of the regimen, and that can add up. “There are not enough resources to support all the other pieces that are required,” Smith with the Campaign to End AIDS said.
In addition to pharma patient assistance programs, a few states like California, Colorado and New York offer subsidized state programs for PrEP. These are meant to support access among uninsured or underinsured patients, who are more likely to be people of color. Some programs cover both the medication and clinical visits and labs, while others only cover one or the other. Most states, however, don’t offer such programs.
In states like Mississippi, where one private payer dominates, “that really determines what people get, what people don’t get,” Mena, the former director of the CDC Division of STD Prevention, said.
Payers often lean toward denials and wait for people to protest.
Amy Nunn, ScD, CEO, Rhode Island Public Health Institute
A recent study estimated that even slight changes in out-of-pocket costs are associated with much higher rates of prescription abandonment. For insured patients, copays for PrEP visits can range from $20 to hundreds of dollars, depending on the plan and provider being seen. Some plans’ deductibles can go as high as $5,000, if not more.
Coverage challenges is something Alex Nelson, PharmD, a specialty pharmacist at Ohio-based MetroHealth, spends a lot of time addressing. It is not uncommon for patients on qualified health plans to face copays for PrEP, according to Nelson.
“There’s definitely a lot of confusion and unnecessary hoops to jump through to get these things paid for,” Nelson said. “We’ve gotten pretty good at our process. You do want to make a case that they’re not going to be able to have an easy conversation with you.”
(Alex Nelson)
“Payers often lean toward denials and wait for people to protest,” Amy Nunn, CEO of the Rhode Island Public Health Institute and professor of public health and medicine at Brown University, told Fierce Healthcare/Uncloseted Media. Anecdotal evidence supports this claim. Data on Medicare Advantage plans, for instance, suggests that 90% of prior authorization requests that get denied are never appealed. At the same time, the vast majority of appeals lead to an overturning of the initial denial.
As a physician, I have no idea what codes are going to be accepted by a person’s insurance company.
Phil Chan, M.D., Chief Medical Officer , Open Door Health
Often, plans require a prior authorization that can be resolved by sending them the information required, Nelson said. But sometimes, the claim gets denied, which requires escalation to a peer-to-peer review. When talking to a plan, Nelson points them to the legal citation that explains the ACA mandate requiring them to cover PrEP. “It’s easier for a person to say no to a piece of paper,” he noted. If they uphold a denial, Nelson submits a written appeal to be reviewed by a payer’s medical director. At that level, appeals are typically approved, he says. But even so, the lengthy process and looming bills could be enough of a deterrent that a patient decides continuing with PrEP is just not worth it.
“For people who are looking to prevent HIV who otherwise seem healthy, each one of these growth bumps presents a great opportunity for people to turn around,” Mena said.
“That creates a public health problem,” echoed Nunn.
Submitting claims for reimbursement as a provider requires a number of procedural and diagnosis codes, which can vary by health plan. “Insurers only accept specific codes,” said Phil Chan, M.D., chief medical officer at public health clinic Open Door Health, run by the Rhode Island Public Health Institute. “As a physician, I have no idea what codes are going to be accepted by a person’s insurance company.”
Pressed for time, providers cannot look up every payer policy to see what codes they accept, Chan added: “I really just take my best guess, and I use those that are commonly used, and frankly I hope they’re covered.”
Will Sharp, a 27-year-old trans man living in Independence, Missouri, spent over seven hours on the phone with his insurance company, Cigna, trying to figure out why his PrEP wasn’t covered when their policy explicitly states it is. “The insurance company said I would have to pay $200 a month, but their policy online said it was covered. My provider at a clinic called Blaque Out spent more than a month going back and forth with my insurance, arguing with them until they realized that they made a mistake,” he said. “It turns out they needed to change something about how the medication was coded in their system. But the whole process took almost two months from when I was prescribed PrEP to when I actually started receiving the medication.” Sharp remains HIV negative.
Similar scenarios have been reported elsewhere.
Cigna did not respond to a request for comment.
Clinicians chasing down reimbursement often face the runaround, like nurse practitioner Kathryn Meyer, DNP, APRN, at MetroHealth, has. Two different people at one health plan could tell a provider different things, leading to a frustrating and time-consuming back and forth. “It’s kind of like calling the airlines,” Meyer said. “I’ve had some people who just make it happen, and I’ve had people who just pass the buck.”
It is not clear if it is intentional. But what is certain is that crucial knowledge is simply missing. “When we speak to people within a pharmacy benefit management or an insurance company, it’s often they’re hearing the information for the first time,” Nelson said about the ACA mandate. Sometimes, they don’t even know what PrEP is: “One person thought I was talking about surgical prep.”
Even employers participating in the U.S. Business Action to End HIV have sometimes discovered they are not complying with the law. “We have had a couple of instances where companies realize that their insurance coverage isn’t providing access to PrEP without cost sharing,” Caroline Jackson, director of the initiative, told Fierce Healthcare/Uncloseted Media.
Some states have gone the extra mile to solidify consumer protections. California prohibits prior authorization for Descovy, a PrEP drug not available as a generic. New York outright prohibits prior authorization for any drugs related to the prevention or treatment of HIV. At least 15 states, none of them in the Bible Belt, require coverage of preventive services with no cost-sharing on top of the ACA.
New Mexico issued sub-regulatory guidance for commercial plans in 2022 requiring them to include specific language in patients’ benefits documents that clearly explains the PrEP no cost-share mandate. The goal is to help patients be aware of their rights, explained Viara Ianakieva, life and health division director at the New Mexico Office of Superintendent of Insurance.
“It’s really important to include detailed information in the benefit booklets,” Ianakieva told Fierce Healthcare/Uncloseted Media. “So if there is a denial by an insurance company for PrEP coverage, at this point it is black and white and it is really easy for the consumer to stand their ground and appeal it.”
In provider deserts, pharmacies hold promise
To increase PrEP use rates among America’s most vulnerable groups, it’s important that the 100 million people—nearly a third of all Americans—who lack access to primary care have options. This is particularly urgent in southern states, where the vast majority of counties are considered primary care shortage areas.
By contrast, nine in 10 Americans live within five miles of a community pharmacy.
“There’s absolutely an opportunity for pharmacists to help increase access to PrEP across the country,” Meg Murphy, PharmD, pharmacy and regulatory affairs manager at Surescripts, said.
“One of the biggest reasons a lot of people of color don’t have access to prevention is they don’t have primary care physicians, don’t have insurance, or are in rural areas,” George Nawas, PharmD, professor of pharmacy at Xavier University, said. “In order to reach these people, and give the prevention medicine before they contract HIV, a pharmacist is a trusted professional for a lot of people who don’t have primary care doctors.”
It’s an opportunity to bring more people into care.
Sara Zeigler, Founder, Courage Forward Strategies
Nearly two thirds of counties with a relative primary care physician shortage fall into the middle or top third of counties by pharmacy availability, Surescripts data shows. A list of the top 10 highest-population counties with such an opportunity includes counties in Alabama, North Carolina, Mississippi and Tennessee.
Natalie Farrior ended up relocating to Durham, North Carolina, for HIV care because there wasn’t enough access where she had been living. She would drive 20 minutes to her clinic, 45 minutes to her closest hospital, and worst case, an hour and a half to get to her primary care doctor. “There wasn’t any community resource for me,” she said. “Even after getting my diagnosis, there was no support. I had to relocate where there are at least some resources.”
(Kate Medley for Fierce Healthcare/Uncloseted Media)
Data from the American Pharmacists Association (APhA) shows 16 states allow pharmacists to prescribe PrEP independently. Another 10 allow it, but only when a provider, typically a physician, formally partners with them.
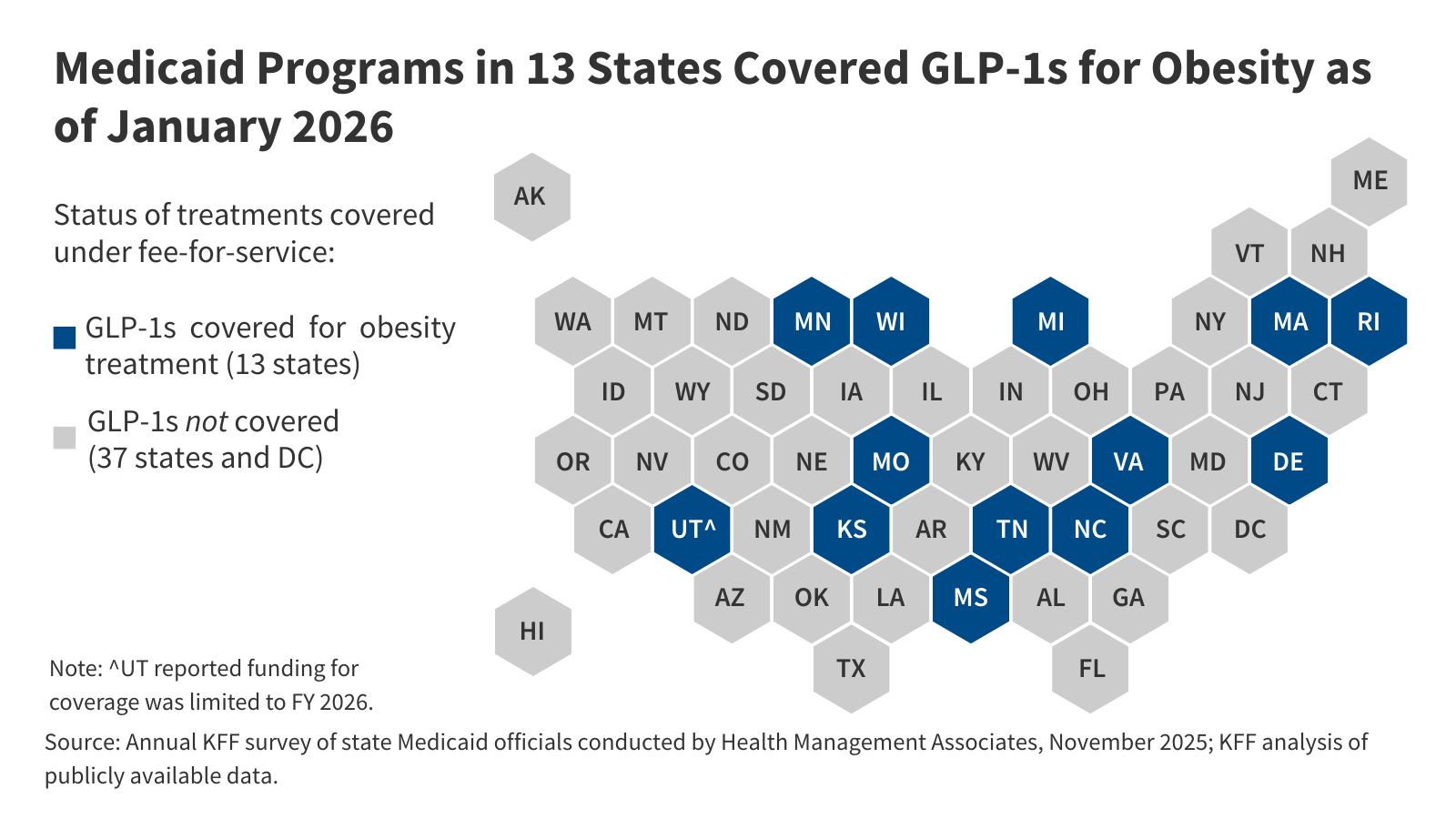
Data shows that living in an area with higher PrEP clinic or pharmacist access significantly increases a person’s willingness to use PrEP. Yet only two Bible Belt states—Arkansas and, as of this summer, Louisiana—give pharmacists independent prescriptive authority for PrEP.
“We’re talking about pharmacies as an entry point, not an endpoint,” Sara Zeigler, the founder of Courage Forward Strategies, a public health strategy firm, told Fierce Healthcare/Uncloseted Media. “It’s an opportunity to bring more people into care. And maybe people who are not currently seeing a physician.”
“That is consistently one of the primary barriers to pharmacists increasing access to HIV prevention care,” echoed E. Michael Murphy, PharmD, senior advisor for state government affairs at APhA, “is ensuring state-based laws and regulations that dictate what a pharmacist is allowed to do are aligned with how pharmacists are educated and trained.”
Zeigler points out that pharmacies can be a less stigmatizing facility because there isn’t one clear reason you are at a pharmacy, and pharmacies have extended hours. “What if I just got chips? What if I got sunscreen?” Zeigler said. “But I happened to see a sign about available HIV prevention services, and I have an opportunity to learn about PrEP.”
Xavier University’s Nawas says that ACT 711, passed in July 2024, authorizes pharmacists in Louisiana to dispense up to a 30-day supply of PrEP. Nawas says that there will be specific training for pharmacists to ensure they are a safe entry point, including how to navigate people who don’t have insurance or a primary care doctor.
“This [ACT] is a way to get more people connected to care by telling them [about PrEP] regardless of money or insurance,” Nawas said.
Remote care eliminates certain barriers, but not all
Another alternative PrEP provision strategy is telemedicine. Not only do virtual appointments eliminate geographic barriers, but they also provide crucial privacy to patients who are not comfortable being seen in person.
“There’s no reason you have to be physically in the same space as the patient unless there’s something wrong. Even if there’s something wrong, a video clinic can often help,” Meyer, the nurse practitioner at MetroHealth, said.
Patients can be seen remotely, get their labs done locally and then have their prescription mailed to them, she explained. All that is truly needed to start on PrEP is a test to confirm they are not HIV-positive. All other labs can wait, Meyer said. She can even start new patients on PrEP virtually, or by phone.
“There seems to be a lot of hesitancy in the medical community to try PrEP on the fly and there doesn’t have to be,” she said.
Melanie Edmonson, a 45-year-old cisgender woman living in Kansas City, Missouri, went to her primary care doctor for PrEP, who referred her to an OBGYN. That doctor then told her to go back to her PCP. “I was surprised how difficult it was to get,” said Edmonson, who at the time was in an open relationship with a bisexual man who was sleeping with other men. Eventually, she found Mistr, an online service that prescribed her the medication.
“If I couldn’t [have gotten] it online, I would probably go back to feeling more terrified of dating and more scared of sex,” she said.
While telehealth is a helpful—and sometimes the only—option for patients, reimbursement for providers can get complicated, according to Neil Parikh, M.D., chief medical officer at Thirty Madison. The company merged with telemedicine and pharmacy delivery startup Nurx in 2022. Nurx offers virtual PrEP services, including counseling, mail-in lab testing and home delivery.
Payers can be hesitant to reimburse home labs. “There’s really patchy coverage at times for services like ours,” Parikh told Fierce Healthcare/Uncloseted Media. “A huge, huge part of being able to maintain your PrEP medication is being able to undergo regular lab testing.” And for many patients, paying entirely out-of-pocket is “challenging.”
Molecular Testing Labs (MTL), an independent lab offering at-home tests, processes about a third of PrEP-related testing in the U.S., James York, the company’s chief commercial officer, told Fierce Healthcare/Uncloseted Media. While most of its business is contracting with 340B-covered entities, MTL still has several thousand commercial claims annually for PrEP. Most of them are not fully reimbursed, or reimbursed at all.
(James York)
MTL, which is in-network with 220 health plans, prioritizes being in-network with as many payers as possible. Yet to date, its applications to be in-network have been rejected by major national plans, York said. MTL’s own analysis of its claims reveals the vast majority submitted to private insurers are rejected as out-of-network.
In 2022, MTL processed 15,695 PrEP tests. Of those, only one-fifth were fully reimbursed by private insurers. For those appealed by MTL, 70% of denials were upheld by private payers. When a claim is denied, MTL bills the patient, so those denials led to nearly half of patients receiving a bill at an average of $94, while MTL still took a loss on those claims, York said. York laid this data out in an open letter, seen by Fierce Healthcare/Uncloseted Media, sent to the Office of National AIDS Policy in 2023.
York believes that large payers keep their lab networks limited to take advantage of the fact that a preventive service must only be covered with no cost-sharing if performed by an in-network provider or an out-of-network provider when no other is available. If a service is performed by an out-of-network lab like MTL, and another in-network lab was available to members, payers can reject MTL’s claims.
“What do the health plans do? They close their networks,” York said. “It’s a business decision for them. They close their networks, and then they don’t let any new labs in.”
“We regularly evaluate our networks to ensure sufficient geographical coverage and services are available for our members,” a major national payer wrote to MTL in a 2023 email, viewed by Fierce Healthcare/Uncloseted Media, rejecting its application to join its network. “We offer contracts based on need…At the present time, we are not expanding our network of laboratory providers.”
When an independent lab like MTL covers nearly a third of all PrEP testing in the U.S., York argued, excluding it from networks hurts both the company and patients.
Envisioning a future with PrEP for all
In addition to telehealth, policy changes could help get more Americans on PrEP. Two-thirds of states in the deep South have not adopted Medicaid expansion and have no state programs for PrEP to support the uninsured. Expanding Medicaid would make the biggest difference to access, advocates like Hiers of AIDS Alabama said. “Our Medicaid in Alabama is so pitiful to begin with,” she said. “That’s the first issue, of course.”
States with both Medicaid expansion and PrEP drug assistance programs had a 99% higher rate of PrEP use relative to states without either in 2018.
“There’s a clear policy path. You advance Medicaid expansion and combine it with drug assistance programs, and what it does is create? This huge uptake in PrEP,” said Will Ramirez, director of public policy and advocacy at the Southern AIDS Coalition. The organization, along with others like PrEP4All, advocates for a national PrEP program, which they say would reduce costs, increase access and reduce coding complexities. The federal Ready, Set, PrEP program distributing free medication to the uninsured stopped accepting new patients in July.
PrEP should have been the standard…This is basic healthcare.
Natalie Farrior, 29, North Carolina
M. Foxworth Blasingame, Ph.D., director of data services at patient engagement platform Healthvana, thinks inadequate behavior change is what’s behind the sluggish progress in HIV prevention today. Extremely effective treatment exists. Yet new HIV cases are not decreasing at an encouraging rate. “It can’t be the science,” Blasingame said. “It’s got to be the behavioral aspect.”
Blasingame, who himself has been on PrEP for more than a decade, thinks lowering the cost of PrEP medications is critical to ending the HIV epidemic. The drug costs him $1,500 a month before insurance and can cost others even more. But PrEP can be manufactured and distributed, at a profit, for about $6 per person per month, according to the testimony of Dr. Robert Grant, one of the pioneers of PrEP research. “That is insane,” Blasingame said. “There is no reason for it to be so expensive.”
There is some movement at the federal level that gives advocates hope. Earlier this month, Medicare announced it would cover PrEP without cost-sharing under Part B. After a request by 63 organizations, including Schmid’s HIV+Hepatitis Policy Institute, USPSTF updated its PrEP recommendation to include long-acting injectable PrEP in 2023.
As a next step, advocates have stressed the need for additional guidance to require insurers to cover the long-acting injectable without cost-sharing. “We are concerned that insurers might just cover one drug… we don’t want them to pick and choose,” Schmid told Fierce Healthcare/Uncloseted Media.
Until something changes, many Americans who need PrEP the most will continue to fall through the cracks.
(Kate Medley for Fierce Healthcare/Uncloseted Media)
“I’m another statistic. I feel let down,” Natalie Farrior, who works in healthcare herself, said. “PrEP should have been the standard. You should be able to go to your clinic, go to Planned Parenthood, and you should be able to get PrEP for free. I understand it’s a factor of the environment I’m in, but this is basic healthcare.”
Dorian McCuller, Natalie Farrior and Sloan Parker are now all undetectable, meaning they cannot sexually transmit HIV to others, and the amount of HIV in their blood is too low to be detected by a test.
Additional reporting done by Spencer Macnaughton, founder and editor-in-chief of Uncloseted Media
Publisher: Source link