Health payers created the prior authorization system as a cost and quality control strategy, ensuring patients receive only the most necessary, evidence-based, cost-effective and quality care. Nevertheless, real-life implementation has shown that prior authorizations often backfire on their original intents, increasing overall care costs beyond what is necessary. It also delays patient care, contributes to physician burnout and hinders operational efficiency.
Additionally, dealing with the administrative workload associated with prior authorizations can be overwhelming, time-consuming and exhausting for providers and billing teams. The sheer volume of paperwork required to navigate the traditional prior authorization system can be exhausting, particularly given the current climate of staff shortages and constantly changing payer policies.
Read on to learn why prior authorizations are crucial to reimbursements and how healthcare organizations can streamline the process using electronic prior authorizations.
What are prior authorizations?
Prior authorizations, also known as preauthorizations, is a process that involves healthcare providers obtaining approval from a health plan for a service or prescription to be delivered to a patient. This approval ensures that the plan reimburses the cost of the service or prescription.
Prior authorizations involve a series of steps. First, healthcare providers confirm the patients’ qualifications for the proposed treatment. Next, they determine whether prior authorization is required. If an authorization is necessary, providers must submit information detailing the patient’s medical history and other administrative information. They also have to submit supporting documents to justify the necessity and appropriateness of the proposed treatment. If the submission meets the prior authorization criteria, the plan approves the request and reimburses the cost of care.
Payers develop prior authorization criteria drawing from medical guidelines, cost considerations, utilization data and other relevant information. However, according to an American Medical Association (AMA) survey, more than one in three providers claim that these rules are rarely or never evidence-based.
Why are prior authorizations required?
Payers created prior authorizations to ensure that the specific service delivered to the patient is medically necessary, appropriate and in line with evidence-based guidelines. It is a cost-and-quality control mechanism. It is set in place so patients only receive the best and most cost-effective care option, optimizing quality while controlling costs.
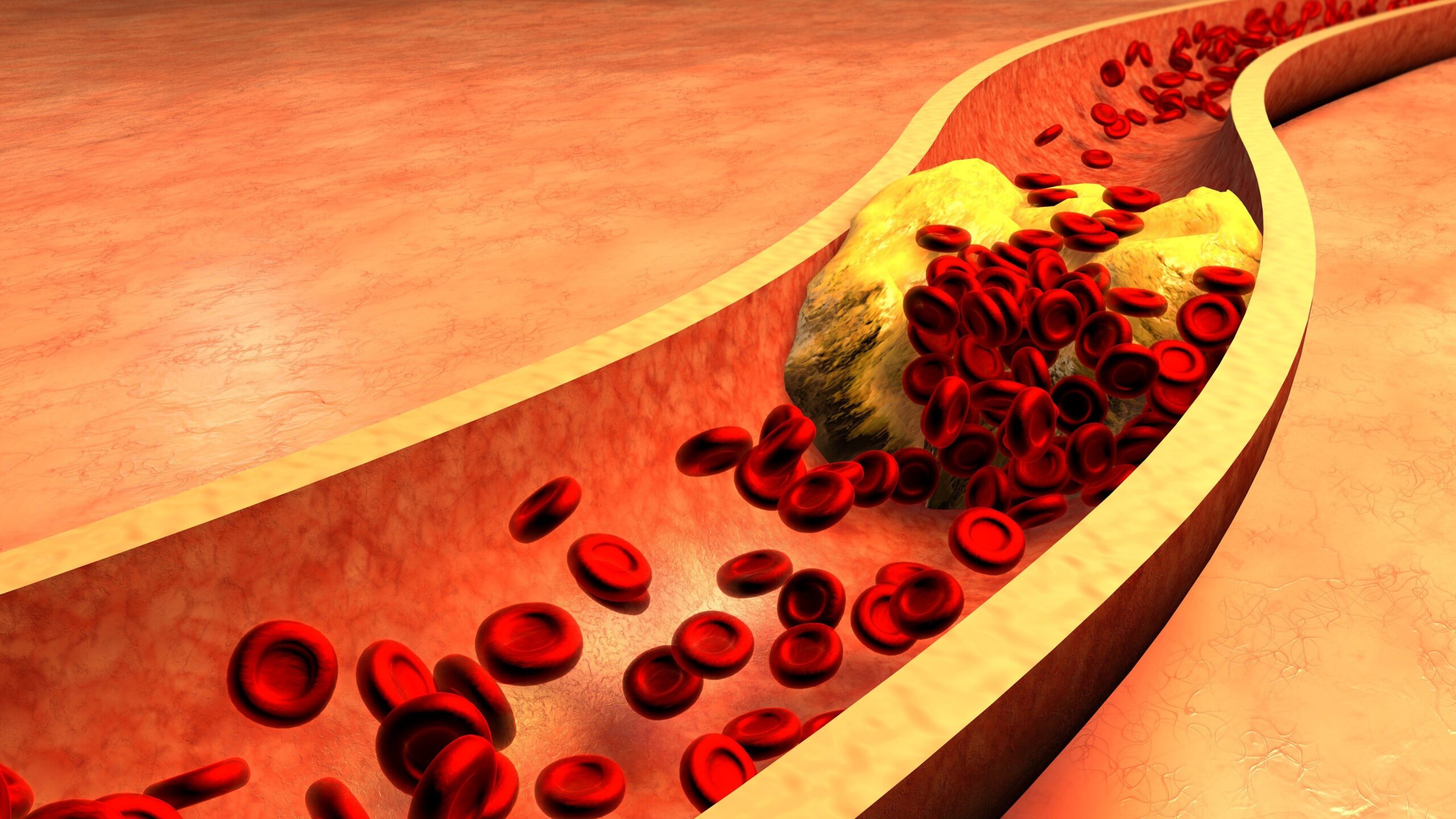
Prior authorizations have been suggested to help manage the cost of care and reduce healthcare spending. Payers employ prior authorizations to prevent the arbitrary prescription of expensive treatments and medications to patients without appropriate justification. For instance, a healthcare provider might prescribe a costly brand-name medication for which a generic and more cost-effective alternative exists.
The prior authorization requirements regulations also ensure that healthcare providers administer evidence-based care and prescribe FDA-approved medications. In cases of off-label use, the requirements help encourage providers only to prescribe treatments supported by high-quality scientific literature. These medications must also meet indications endorsed by recognized sources such as the American Hospital Formulary Service Drug Information (AHFS-DI).
Challenges with traditional prior authorization methods
For many providers, dealing with prior authorization is an endless journey of starting, completing and revising paperwork. This process presents administrative challenges, leading to a significant waste of time and resources. An AMA survey found that 86% of physicians have reported that prior authorization increased healthcare resource usage.
Healthcare providers frequently allocate a large portion of their daily schedules to addressing prior authorizations. This practice takes staff time and effort that could otherwise be dedicated to providing high-quality patient care. According to an AMA prior authorization survey, healthcare providers spend about 12 hours working on 43 prior authorizations weekly. Not to mention that over one in four providers report that these prior authorization requests often or always end up being denied.
These experiences with traditional prior authorization methods have severe consequences for healthcare providers. They lead to increased physician workload, burnout, and lost time and productivity.
For patients, the time required to process manual paperwork can be a frustrating roadblock to accessing timely care. A convoluted prior authorization process also adds extra hurdles to working with different healthcare specialists for patients with multiple chronic conditions. Consequently, processing prior authorizations through traditional methods could lead to delays in care and even treatment abandonment.
The impact on patient outcomes isalso quite significant. According to the AMA, more than nine out of 10 doctors report negative effects due to prior authorizations.
Additionally, payer policies are constantly changing, compounding this issue. It’s hard for providers to stay up-to-date and ensure submissions are accurate. These new changes are often unannounced, making it more likely for healthcare providers to make prior authorization requests based on outdated rules. As a result, many of these submissions are instantly rejected.
Challenges with traditional prior methods point to one fact: the need for a more efficient prior authorization system is evident and urgent.
Why healthcare providers should use electronic prior authorizations
Electronic prior authorization entails systems or solutions that streamline the process of obtaining approval for proposed medical procedures, services and medications to be delivered. These systems enable healthcare providers to initiate authorization requests electronically, eliminating the need for manual paperwork processing. They are designed to improve operational efficiency, reduce healthcare providers’ administrative burden and ensure patients receive care as early as prescribed.
Alicia Pickett, Senior Product Manager at Experian Health, says, “As healthcare providers face increasing administrative demands, automating prior authorizations is no longer just an efficiency measure—it’s a necessity. By streamlining this process, we enable providers to focus on what matters most: delivering timely, high-quality care to their patients.”
Overall, electronic prior authorizations connect payers’ objective of only remunerating high-quality, appropriate and cost-effective care and providers’ aspiration to bypass excessive procedural prerequisites for reimbursement. They also help ensure patients enjoy seamless and timely healthcare encounters that culminate in favorable clinical outcomes.
The benefits of electronic prior authorization solutions
The traditional prior authorization workflow can be tedious, time-consuming and error-prone. Enter electronic prior authorizations. Its unique capabilities offer many advantages for hospitals, healthcare providers and patients.
Neeraj Joshi, Product Director at Experian Health, says, “The true value of electronic prior authorizations lies in its ability to remove barriers to care. By reducing approval times and minimizing paperwork, patients receive faster access to the treatments they need, ultimately leading to better outcomes and fewer delays in critical care.”
Here are some benefits of using electronic solutions to address prior authorization hurdles.
Reduced administrative burden
Prior authorization can be lengthy and frustrating when healthcare providers have to gather, review and complete hundreds of pieces of paperwork weekly. Electronic prior authorizations accurately and efficiently take care of these burdens in a way that human efforts cannot replicate.
Improved operational efficiency
Electronic solutions for prior authorizations are a partner tool that helps hospital management allocate resources appropriately. They can also help reduce staff workload and workflow, even amidst staff shortages. By freeing healthcare providers and staff from the time-consuming task of handling prior authorization paperwork, they can focus more on enhancing patient experience, care and satisfaction. As a result, hospitals have a more productive, less stressed and efficient workforce.
Reduced claim denials
Errors in the prior authorization process are a leading cause of claim denials, particularly when hospitals use traditional methods. Electronic authorizations help reduce the risk of claim denials by ensuring accuracy and completeness at every step of the submission process.
Improved patient experience and outcomes
Traditional prior authorization methods lead to costly care delays and frustrating patient encounters with the healthcare system. On the other hand, electronic accelerates time to care delivery, reducing the likelihood of patients experiencing adverse effects.
Increased hospital financial resources
By automating the prior authorization stage, healthcare organizations can speed up the entire claims and revenue management process. This accelerated system also helps reduce claim denial rates and boosts reimbursement rates. As a result, cash flow improves, ultimately strengthening their financial standing.
Key features of prior authorization software
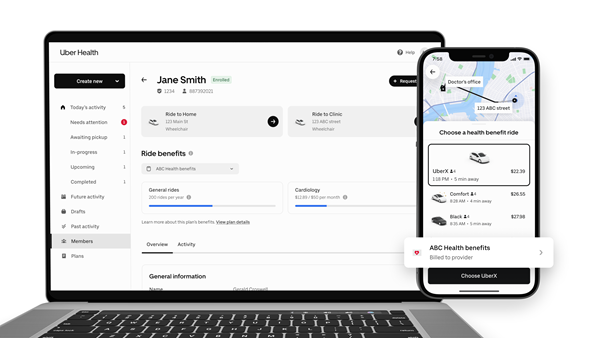
Experian Health’s prior authorization software, Authorizations, is an integrated online service that automates the inquiry and facilitates the submission processes for prior authorizations. The system automatically fills in payer information, and users are only infrequently prompted to make inputs.
Key features of the prior authorization software include:
- Knowledgebase: Authorizations can access real-time and up-to-date prior authorization requirements and criteria in the National Payer Rulesets.
- Submissions support: The software guides users to the appropriate website and presents patient data in an efficient format so that users can create clean submissions.
- Enhanced workflow: It works with dynamic work queues, which provide an instant view of the prior authorization status and guide users through any pending tasks.
- Postback: Users can send information about authorization status to the health information system (HIS) and practice management systems (PMS).
- Image storage: Images of payer responses can be received and stored securely in the software’s integrated document imaging system.
- Reconciliation: The software offers insights into and helps resolve authorization variances, allowing staff to take proactive steps to prevent denials and appeals.
Electronic prior authorization solutions are a valuable time- and resource-saving investment for stakeholders in hospital revenue management. According to the Council for Affordable Quality Healthcare (CAQH), the healthcare industry could save around $494 million annually by using them. In addition, providers can save 11 minutes per prior authorization transaction with electronic solutions.
Additionally, electronic prior authorization software creates a win-win situation for healthcare providers and payers: Payers only release payments when necessary and hospitals get steady, adequate cash flow to meet the operational expenses of delivering quality care.
Find out how Experian Health’s electronic prior authorization software, Authorizations, helps healthcare organizations achieve faster reimbursement rates.
Publisher: Source link