On May 22, the House passed a budget reconciliation bill that makes significant changes to the Medicaid program, including adopting a national work requirement for certain people covered by Medicaid. The new requirements would apply to adults eligible through the Medicaid expansion and would require them to work 80 hours or more per month, engage in work-related activities, or be in school half time. Certain individuals, including parents of dependent children and individuals who are “medically frail,” (defined as those who have a physical, intellectual, or developmental disability, a substance use disorder or “disabling” mental disorder, and those with “serious or complex” medical conditions), would be exempt from the requirements.
Under the House-passed bill, whether an individual is meeting the work requirements would be assessed at application and at renewal. Adults applying for Medicaid would have to meet the requirements or qualify for an exemption at least in the month preceding their application and could be required at state option to meet the requirements for more than one consecutive month. Adults enrolled in Medicaid expansion coverage would have to meet the requirements for at least one month between 6-month eligibility determinations, or more frequently at state option.
Text of the Senate version of the reconciliation bill, released on June 16, also includes a Medicaid work requirement similar to the provisions in the House bill, though it makes some changes to who is exempt from the requirement, notably narrowing the exemption for parents to those whose children are ages 14 and younger.
The Congressional Budget Office estimates the Medicaid work requirement provisions in the House bill would reduce federal spending by $344 billion over ten years, and increase the number of people without health insurance by 4.8 million. Based on experience with work requirements in Arkansas, where 18,000 enrollees lost Medicaid coverage following implementation of work requirements, many adults are expected to lose coverage because of difficulty navigating the reporting requirements and proving they worked the required hours or qualified for an exemption.
This analysis builds on prior analysis of the work status of Medicaid enrollees and uses data from the Survey of Income and Program Participation (SIPP) to model the impact of the work requirements in the House-passed bill. It includes adults on Medicaid who are not receiving disability income, are not also enrolled in Medicare, and are not parents of dependent children in states that had adopted the Medicaid expansion as of December 2021, as these adults are likely to be subject to the new requirements. Specifically, the analysis examines the work status of these Medicaid adults to assess whether they would meet the 80+ hours per month requirement and identify the reasons why individuals may not be meeting the requirement. It also examines work status throughout the year for this group to determine whether adults who meet the work requirement by working 80 or more hours in one month continue to meet the requirement in subsequent months.
KFF Analyses of Medicaid and Work
To understand the impact of Medicaid work requirements included in the budget reconciliation bill being debated in Congress, KFF has undertaken two difference analyses using different data sources. Below describes the differences between these analyses.
Current Population Survey (CPS): Study population includes adults with Medicaid who do not receive disability payments or who are not enrolled in Medicare. Analysis measures the share who worked full-time or part-time, regardless of the number of part-time hours worked. Among those who did not work, examines the reasons why they did not work. Work status is measured for the full year and includes those who worked the entire year as well as those who worked part of the year. The time period for the analysis is 2023. In addition to national estimates, CPS allows for state-level estimates for some measures.
Survey of Income and Program Participation (SIPP): Study population includes adults with Medicaid who do not receive disability payments, who are not also enrolled in Medicare, and who are not parents of dependent children. Analysis measures the share of adults who work 80 or more hours in a month, and for adults who did not work 80+ hours, the reasons why they did not work the required hours. The time period for the analysis is June 2022 (SIPP captures work status on a monthly basis).
Monthly Work Status
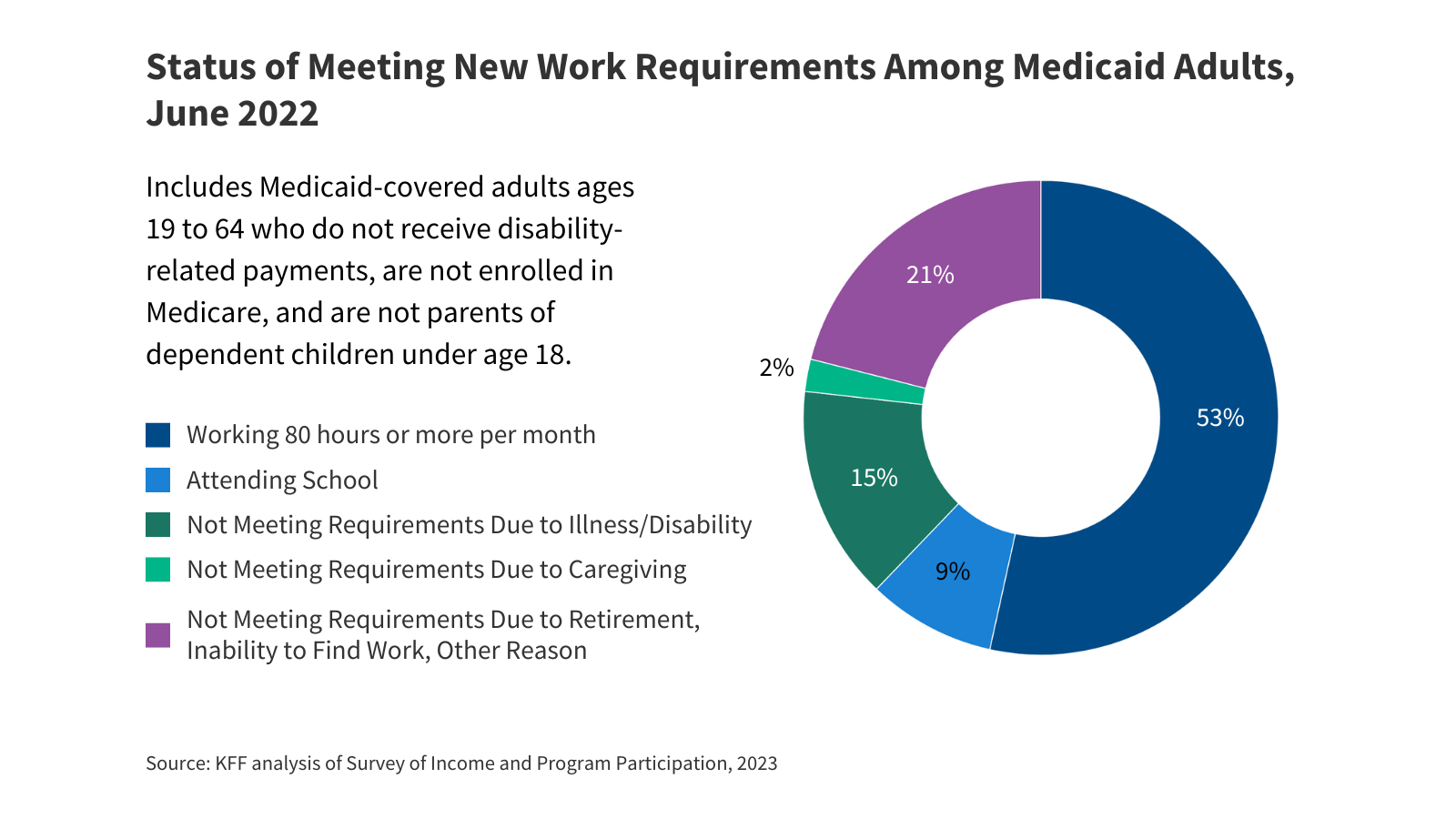
Among Medicaid adults who would be subject to the work requirements in the House-passed reconciliation bill, nearly eight in ten either met the requirement to work at least 80 hours or did not meet the requirement for a reason that would likely qualify them for an exemption. Over half (53%) worked at least 80 hours in the month analyzed (June 2022) and 9% were attending school (Figure 1). Nearly one in five (17%) of adults did not work 80 or more hours because of illness or disability (15%) or caregiving responsibilities (2%), reasons that could qualify them for an exemption from the requirement. However, about one in five (21%) Medicaid adults were not working or did not work enough hours to meet the requirement for reasons, including the inability to find work or to work more hours, retirement, or having been laid off, that would put them at particular risk for losing coverage if the new requirements go into effect.
The share of adults who would meet the new requirements or qualify for an exemption varies by age. Over seven in ten (72%) of young adults ages 19-27 were working 80 or more hours (48%) or were in school (24%) and would have met the requirements, the highest share of any age group. An additional 7% reported having an illness or disability (Figure 2). A slightly smaller share (66%) of adults ages 27-49 would have met the requirements while one in five would have qualified for an exemption based on health limitations or caregiving responsibilities. Adults ages 50-64 were least likely to meet the requirements, with less than half (48%) working 80 or more hours in the month. However, nearly a quarter (24%) of these adults were not meeting the requirements for reasons that would likely qualify them for an exemption.
Adults ages 50-64 are at greater risk of losing Medicaid coverage for not meeting the new requirements. Adults who are not working 80 or more hours in the month and who do not appear to qualify for an exemption because they cite an inability to find work, retirement, or other reasons for why they are not working are at the greatest risk of losing coverage if the work requirements are implemented. Nearly three in ten (29%) Medicaid adults ages 50-64 are not meeting the work requirements and do not appear to qualify for an exemption (Figure 2). While similar shares of adults ages 50-64 compared to other age groups cited being unable to find work or other reasons for not meeting the work requirements, over one in ten (11%) said they had retired. Among adults who said they retired, 28% reported having a disability. Because of their age and physical limitations, these adults may face particular challenges trying to reenter the workforce, if they don’t meet reporting requirements to qualify for an exemption.
Work Status Throughout the Year
About 10% of Medicaid adults who meet the requirement to work 80+ hours in a month do not continue to meet the requirement for all of the following six months. Under the requirements in the House-passed bill, states must confirm that individuals meet the work requirements at application and every 6 months when eligibility is redetermined (or more frequently at state option). States would be required to “look back” at least one month between 6-month eligibility periods and could choose to “look back” more consecutive or non-consecutive months to verify compliance. While 44% of Medicaid adults who met the requirement to work 80+ hours in June continued to meet the requirement in all six months from July to December, 4% met the requirement for 4 or 5 months and 5% met the work requirement for only 1, 2, or 3 months during the 6-month period from July to December. Depending on how states operationalize the “look back” period, the month-to-month volatility in hours worked could lead to increased coverage loss, but even individuals who continue to meet the requirement could still lose coverage if states require monthly verification.
Similar to previous analyses, this analysis shows that a majority of Medicaid expansion adults who would be subject to the work requirements in the reconciliation bill are working 80 or more hours in a month, and most are working those hours consistently over a six-month period. Many adults who do not meet the work requirements are attending school or have an illness or disability that limits their ability to work and would, therefore, appear to qualify for an exemption from the work requirements. Nevertheless, these adults are at risk of losing coverage if they are unable to navigate reporting requirements established by their state. Expansion adults ages 50-64 may be at greater risk of losing coverage under the new requirements because they are less likely to work 80 or more hours in a month or to qualify for an exemption.
Methodology |
Data for this analysis are from the 2023 Survey of Income and Program Participation (SIPP), which covers calendar year 2022. The analysis focuses on the working patterns of individuals in the month of June 2022 who:
To identify reasons for not meeting work requirements, defined as working more than 80 hours per month, responses were combined from several questions, including reasons for not working and reasons for working part-time. Furthermore, to assess work status across a six-month window, individuals who met the work requirement in June were then followed from July through December to examine how their work status changed over time. |
Publisher: Source link